The post MMC and the New Hospital Programme: unlocking the limitless potential of prefabrication appeared first on Without Limits.
]]>The post MMC and the New Hospital Programme: unlocking the limitless potential of prefabrication appeared first on Without Limits.
]]>The post Healthy hospitals for a healthy planet: balancing carbon versus space appeared first on Without Limits.
]]>Here, we share what this vital but challenging new standard means for the industry – and why a delicate balance must be struck between minimising carbon and maximising space.
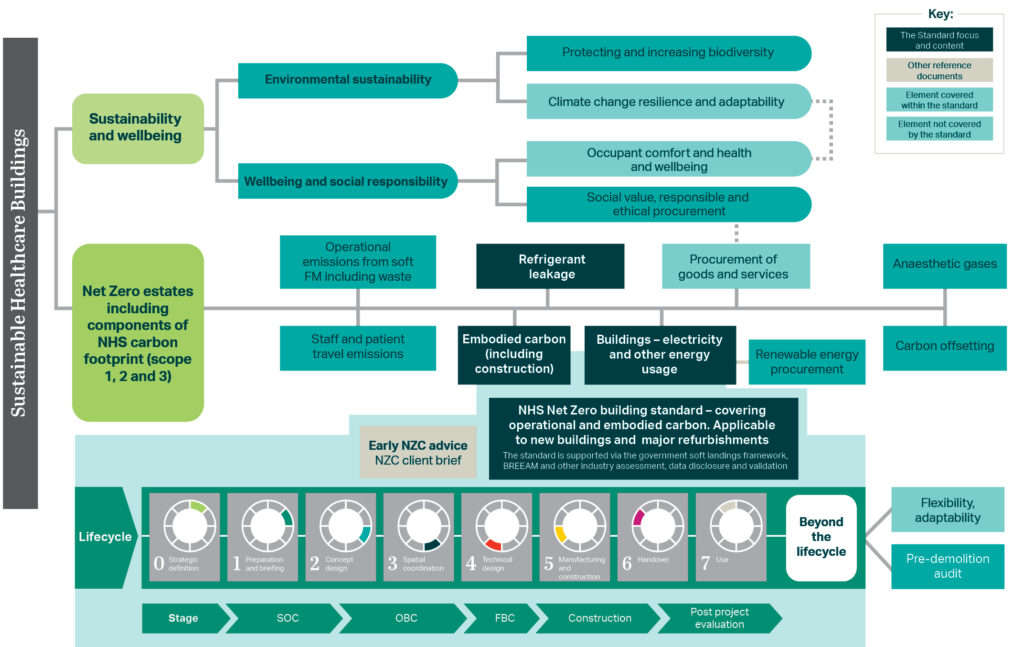
In February 2023, the UK’s National Health Service (NHS) issued the UK’s first Net Zero Building Standard for delivering net zero carbon healthcare buildings. In doing so, it created a blueprint – and set a challenge – for healthcare providers around the world to follow.
The Standard is part of the NHS’s commitment to become net zero carbon by 2045. Decarbonising the NHS is a mammoth task. More than 3000 buildings fall under its stewardship, contributing 4-5 per cent of the UK’s total carbon emissions each year.
Why now?
Climate-change-related health problems are rising, laying an added burden onto an NHS already under deep strain. The NHS’s decision to be the first health system to embed a net zero target into legislation (via the Health and Care Act 2022) is bold and takes a proactive approach towards urgently mitigating climate change.
The impact of rising temperatures is proving vastly expensive to manage. The Royal College of Physicians reported that the 2003 heatwave cost the NHS £41.4 million. The NHS spends over £50 million a year on carbon permits to offset its CO2 production. The costs of failing to decarbonise one of the UK’s biggest institutions are now simply too high from legal, financial, social and health perspectives. In short, climate change threatens the NHS’s viability.
Why develop a standard for new buildings?
Healthcare buildings are energy and resource-hungry spaces, running 24/7, 365 days a year. Decarbonising new buildings can only shave a small slice off the NHS’s total carbon emissions. Much more work is needed to reduce carbon and energy used by existing building stock, and the NHS’s scope 1, 2, 3 and travel emissions, as outlined in the graphic below.
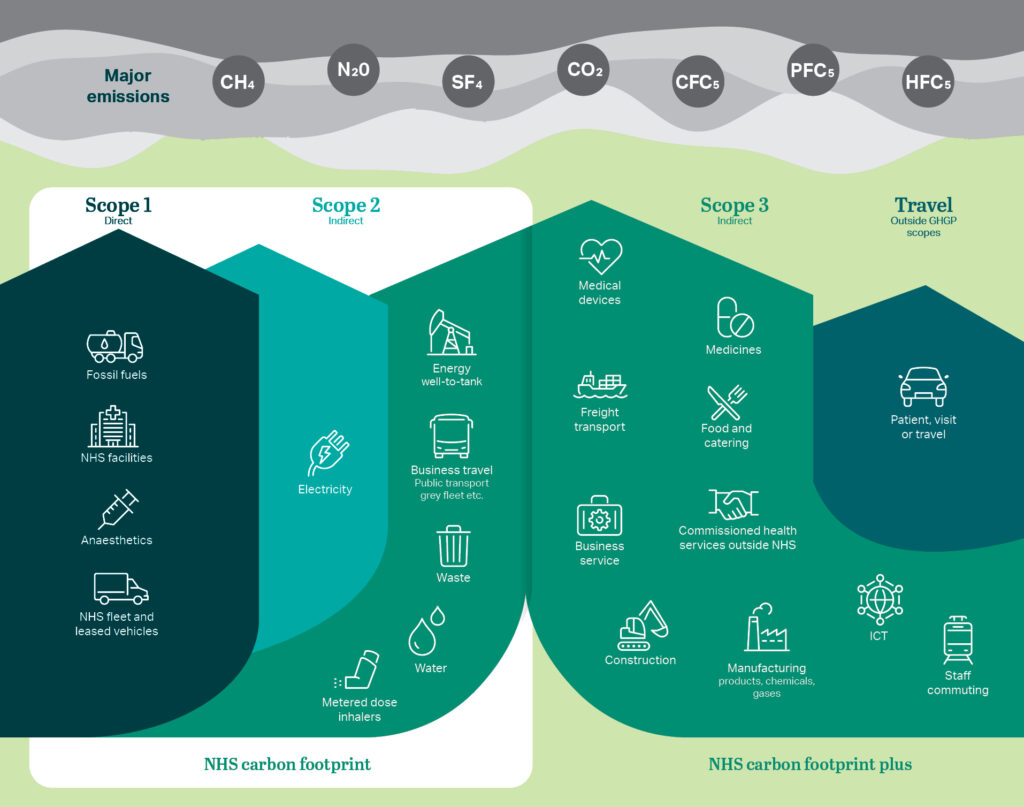
However, by making it mandatory for new buildings to be net zero carbon, the NHS is furthering its decarbonisation mission through implementing incremental improvements. In time, as older buildings are decommissioned, a more efficient estate will be created.
How can it be achieved?
The Standard applies to all investments in new buildings and major upgrades to existing facilities from October 2023. It provides technical guidance to develop sustainable, resilient, and energy efficient healthcare buildings.
The Standard sets out an approach to low carbon building design by setting performance criteria for key design drivers that include:
- Minimum performance targets (MPTs) for construction U-values and building services plant efficiencies.
- Setting carbon limits for operational energy on a departmental basis and embodied carbon for the major components of the building.
- Crucially, it requires the reporting of whole life carbon – both to create an accurate picture of the carbon output of a building and to inform and refine future iterations of the Standard.
The challenges: applying the NHS Standard to our hospital designs
Creating a sustainability standard for inherently power-hungry buildings is immensely difficult – not least when it must be integrated alongside other best practice guidance for achieving high quality healthy, sustainable buildings.
The Standard is designed to be adaptable and recognises hospitals’ high base energy demand. The methodology will undoubtedly need to improve with time as learnings from different hospitals emerge. It is evolving and being actively tested via our projects.
As designers, our biggest challenge is creating a balance between ensuring we achieve sustainability goals, within the NHS’s project budgets – without impacting the critical clinical delivery pathways and outcomes within the flexibility needed for future change.
Cambridge Cancer Research Hospital

Right now, we are testing the implications of net zero design on live projects, including the Cambridge Cancer Research Hospital (CCRH).
A collaboration between Cambridge University Hospitals NHS Foundation Trust, the University of Cambridge, Cancer Research UK, and commercial partners, the 27,083m² project is a nine-storey standalone building.
Due for completion in 2026, the hospital will be a key centre of care and translational research for cancer patients and an early example of the NHS’s net zero carbon building standard in practice. The average hospital on the neighbouring Addenbrooke’s Hospital campus uses around 405-470 kWh/m2 of operational energy a year; CCRH’s operational energy target will be more than half this consumption, at 200 kWh/m2 a year.
To achieve the ambitious carbon reduction target for CCRH, we are focusing on the following:
- Being lean – reducing energy demand through passive design measures and optimising clinical space design.
- Improving fabric – designing a highly insulated, high-performance building envelope.
- Decentralised plant – minimising service runs and providing plant space near the specific clinical functions.
- Creating clean onsite energy – onsite Solar PVs on a biodiverse green/blue roof.
- Efficient use and reuse of heat and cooling – through integrating ASHP and GSHP technologies.
- Measuring through a Whole Life Cycle Carbon approach.
Greener buildings, healthier lives
New healthcare buildings stand at the intersection between health, technology, and design. With hospital buildings being vastly energy intensive in their operation, construction, and eventual decommissioning, creating a net zero carbon hospital without financial carbon offsetting is unlikely to happen. The Standard recognises this and aims to offset its overall carbon footprint at an institutional level, rather than individual buildings.
Decarbonising one of the biggest institutions in Europe, and indeed the world, is an incredibly difficult task: but this does not mean we should not rise to the challenge. The NHS has already reduced its emissions by 30 per cent since 2010; this is just another step forwards in making a low-carbon NHS a reality. The decarbonisation of NHS building design is a significant step forward in improving public health – and a great example of exactly what this institution was created to achieve.
The post Healthy hospitals for a healthy planet: balancing carbon versus space appeared first on Without Limits.
]]>The post Designing the UK’s community diagnostic centres appeared first on Without Limits.
]]>Building community diagnostic centres (CDCs) is a priority for NHS England. Right now, thirteen new CDCs are being launched across the country – part of a £2.3 billion plan to establish up to 160 centres by 2025.
The primary goal is to reduce waiting times for NHS patients who need non-urgent care. The NHS England elective waiting list stands at around 6.4 million people. As of December 2023, 337,450 people in England have been waiting more than a year to receive care.
Historically, diagnostic care – used, for example, to identify and monitor cancers and long-term health issues – would be the preserve of acute hospitals in larger towns and cities. Today, diagnostics are increasingly moving into separate buildings, off acute sites and even into temporary locations. This is to meet the needs of ageing, less mobile populations and to also achieve a key part of the NHS Long Term Plan, which includes the goal to deliver more care outside of major acute hospitals.
Tailoring design to meet local needs
Each project is highly individualised based on the NHS Trust, the geography, and local need. Where cost savings can be made largely depends on the client’s drivers.
Available locations vary widely, and designers must consider a proposed project’s interaction with and impact upon adjoining buildings. Some projects join existing NHS estates; others repurpose existing commercial space. For example, University Hospitals Dorset NHS Foundation Trust created a CDC using vacant shopping units in the Dolphin Shopping Centre, which has had the added benefit of driving footfall to the centre.
As technology evolves, building design must evolve with it
Fit-out equipment depends on the diagnostics being carried out on site. These often include imaging equipment, computed tomography (CT) scanners and MRI scanners. As these technologies advance, a CDC must be designed to be adaptable to meet changes in service delivery. This means from the earliest stages, consideration should be given to slab-to-slab heights, lift provision and the ability to expand the space.
In multi-storey buildings, the sheer weight of imaging equipment theoretically calls for diagnostic rooms to be situated on the ground floor. The challenge is that diagnostic equipment typically requires large spaces, which are often found in healthcare buildings above-ground. This means sometimes the building grid does not ideally stack: early space planning of key adjacencies helps overcome this issue. Mitigation of vibration is another key design consideration.
One healthcare technology evolution which is shaping the design of CDCs is the growing shielding requirements of imaging equipment. MRI scanners, for example, require a Faraday cage – an enclosure used to block electromagnetic fields – as well as stainless steel reinforcement to enhance the quality of the imaging that is produced. These are unavoidable cost pressures that should be designed and priced in from the outset.
Addressing safety and capacity challenges in CDC design
Electrical and data infrastructure usually must be upgraded on existing sites to enable these facilities to operate, as many Trust estates are already at, or over maximum capacity with their electrical load.
Incorporating MRI equipment into a building has the added challenge of safely installing quench pipes, which safely discharge helium gases from the scanners and out of the building. In turn, the heat loading associated with this imaging equipment is so extreme that it can skew the mechanical, electrical and plumbing (MEP) design and, if not considered at the earliest design stages, potentially cause significant problems further down the line.
The future: could CDCs transform the UK’s healthcare system?
CDCs present a trifecta of obstacles: cost, decarbonisation, and delivery challenges must all be considered. Encouragingly, we are already seeing solutions and completed projects emerge that are overcoming these obstacles – and promptly cutting down local NHS waiting times in the process.
Case study: Ambulatory Diagnostic Centre, West Middlesex University Hospital
Chelsea and Westminster Hospital NHS Foundation Trust is constructing a £73 million Ambulatory Diagnostic Centre (ADC) at West Middlesex University Hospital.
This is the largest capital project that the Trust has ever undertaken and includes a £15 million capital grant from NHS England.
The new state-of-the-art facility will provide cancer, renal and imaging services for the residents of Hounslow, Richmond, and Ealing, ensuring that people can access tests and treatment more quickly and closer to home.
Cancer and renal disease are some of the biggest health issues among the local population. The ADC will double capacity for these services, ensuring that the local community can access treatment locally. It will also help reduce pressure on urgent care services at the main hospital, by caring for non-urgent patients at the ADC.
The centre will include an education facility for staff, which it is hoped will aid recruitment and retention of staff within the local community.
The project is expected to be complete by the end of 2026. AECOM is providing several services for the project – acting as lead designer, architect, civil and structural engineer, fire engineer and BREEAM advisor.

Case study: Northamptonshire CDCs
Northamptonshire NHS Group is set to receive nearly £17 million in funding to establish two CDCs: one in Corby and one in Kings Heath, Northampton.
At present, waiting times for routine non-urgent specialist tests such as MRI and CT in the University Hospitals of Northamptonshire NHS Group, which are developing the sites, can be up to 20 weeks for an MRI and 13 weeks for CT tests.
The new CDCs are expected to quickly cut waiting times for these procedures once they become operational this year, operating for 12 hours a day, seven days a week. Once fully operational, the two CDCs will be able to deliver at least 90,000 additional tests each year, including 16,000 additional MRI scans and 24,000 additional CT scans.
AECOM were appointed as architects, project and cost managers, and both CDCs are expected to be operational in 2024. In the meantime, routine tests are being carried out in mobile units to try and alleviate demand for care.

Cost model: new-build diagnostic centre
The cost model is for a newly built three-story diagnostic centre in the South-East of England, boasting an internal floor area of 4,600 square metres.
The cost estimate is based on data from 2Q 2023 and includes provisions for Group 1 and Group 2 furniture, fixtures, and equipment installation. However, please note that the costs do not include demolition, utilities diversions/upgrades, client design and construction contingencies, optimism bias, client-supplied equipment, professional fees, S106 contributions, surveys, and VAT recovery.
It is important to note that rates may require adjustments to reflect specifications, site conditions, procurement routes, and project timelines.
Click here to download the cost model.
This is an abridged version of an article that was first published in Building magazine. You can read the full article by clicking here.
The post Designing the UK’s community diagnostic centres appeared first on Without Limits.
]]>The post A new vision for mental health facilities appeared first on Without Limits.
]]>The 2019 Royal Commission into Victoria’s Mental Health System final report called for an ambitious reform agenda with more than 65 recommendations to improve the state’s mental health and well-being system. The expansion of flexible mental health infrastructure is the centrepiece of significant investment commitments from the Victorian State Government and is shining a light on the need for modern facilities that support recovery-focused treatment and provide consumers with an appropriate level of autonomy over their environment.
Over the last two years, the Victorian state budget has committed more than $AUD 5 billion (US$3.4 billion) to support better mental health outcomes. AECOM is currently engaged on several mental health projects, including the secure forensic mental health facility, Thomas Embling Hospital. The 136-bed facility is undergoing expansion and refurbishment, providing an additional 82 beds by the end of 2024. The hospital provides treatment and care for people living with a serious mental illness who are in, or at risk of entering, the justice system. The $AUD474 million expansion will address critical bed shortages, providing 82 new secure mental health beds, including a new dedicated women’s precinct, a medium security men’s facility and a new entry complex. AECOM is providing multidisciplinary engineering services for the project, working closely with Guymer Bailey Architects and MAAP Architects.
In this article, we share learnings from the design and delivery of mental health facilities in Victoria and explore the key considerations that make these facilities unique from any other health facility.
Co-designing a better future
As design professionals, we are responsible for interpreting and responding to community insights to provide better spaces that support recovery.
Modern-day mental health facilities are an important part of our community, and their design is evolving with greater recognition of recovery-focused outcomes. Learning from those with lived experiences through the ongoing co-design of facilities is integral to the evolution of mental health care and ensuring the needs of consumers are met. For example, during the co-design process, consumers can share aspects of a facility where design solutions could improve their experience, or they could share their personal experiences, such as feelings of fear and confusion when arriving at a facility and the key design elements that could improve the experience.
Through co-design, we gather their unique insights – what were the pressure points, what was good and how could it be better? Their perspective is essential to ensuring our facilities are fit for purpose.
The design of mental health facilities is critical in providing a safe and rehabilitative environment for consumers, and while from the outside, facilities may appear to be similar to other buildings, they are highly bespoke with every aspect, from design to material selection and audio-visual solutions, considered.
Six key considerations
- Safety is the core design principle: safety is at the heart of the design process to ensure the wellbeing of consumers and staff. Safety is prioritised across every design element and impacts everything from electrical solutions and fire safety interventions to ceiling heights to reduce risks of self-harm. For example, a higher level of acoustic treatment is required in mental health facilities to minimise stress incurred from noise in adjacent spaces. When considering security design, it’s important to take a mitigative approach using passive systems, which are unobtrusive and respectful of privacy while prioritising consumer and staff safety.
- Designing for flexibility: it’s critical to design facilities to be flexible and adaptable to cater to changing models of care and to reduce the impact on facility operations and unnecessary disturbances to consumers. For example, floor-to-floor heights will need to be coordinated with building services to make it easier to adapt spaces in the future. This requires a highly integrated design between engineering disciplines and architects.
- Sustainability and access to nature: the environment has an important role in enabling a salutogenic approach to health and wellbeing. A healthy and comfortable indoor environment is widely accepted to support positive health outcomes for consumers and staff. Access to daylight and improved indoor air quality is vital to achieving this and can be supported using anti-ligature operable windows to help consumers control their environment. Providing consumers with a connection to nature through biophilic design solutions that use natural materials and providing courtyard areas and visual access to the landscape through views of water and green spaces can also support recovery. The use of temperature control can also be beneficial to help reduce aggressive behaviours and encourage good sleep hygiene, while the use of circadian lighting can be used to support health and wellbeing by mimicking natural lighting to align with our biological clock.
- Technology: plays an important role in recovery. Internet connection and web-based communication platforms can provide consumers with a sense of connection to friends, family, and support networks beyond the mental health facility and access to training and development programmes. These connections form part of an integrated approach to treatment and support their reintegration into society and ability to lead a meaningful and contributory life. Audio-visual technology solutions, such as sensory rooms with fibre-optic star ceilings and wall projections create immersive experiences for consumers and are designed to aid rehabilitation.
- Designing for infectious disease: the coronavirus pandemic has fundamentally changed how we design buildings. We are now acutely aware of the need to control the spread of infectious diseases, and how this will inform design outcomes in future. In practice, this could be designing specific wards that can operate safely in pandemic mode or be more easily adapted to suit pandemic operational requirements. This is particularly critical for mental health facilities where consumers cannot be easily transferred to other facilities due to specific safety and security requirements or where disruption to one’s environment may impact recovery outcomes.
- Embed your costing in the process: mental health facilities are inherently complex. What appears as a regular building component is rarely as it seems, for example, plywood backing behind walls for reinforcement, anti-pick caulking around fittings, and tamperproof and anti-ligature fixtures and fittings all add a premium cost. Every aspect requires more or special materials or time to achieve the level of robustness needed. This means there are significant cost risk factors across every design element, and they must be tracked throughout the project to reduce the risk of going over budget.

A solution for all
Mental health projects require meticulous planning and delivery experience. New technology and models of care are driving better outcomes for consumer recovery, and how our buildings transform over time requires both an agile mindset and a considered approach. Innovative ideas are important to push the industry forward and drive better care, but to be successful in a mental health setting, a thorough understanding of the unique sensitivities and pressure points is vital to creating a built solution that meets the needs of consumers, their families, and staff alike.
The post A new vision for mental health facilities appeared first on Without Limits.
]]>The post A holistic approach to designing cancer care facilities appeared first on Without Limits.
]]>The UK is home to some of the most innovative state-funded cancer treatment centres in the world. However, the NHS is under immense strain: record numbers of people are coming forward for cancer tests, with almost a quarter of a million referrals per month in 2022, according to NHS data. This is triple the number of referrals reported in 2020, when the coronavirus pandemic meant people were often reluctant to attend hospitals or to visit their GP practice.
This means cancer care centres are dealing with all-time high levels of referrals and patients, at a time when coronavirus and its attendant risks is still ongoing. Those commissioning cancer facilities are tasked with the challenge of delivering high-quality spaces which are sensitive to patient needs, while incorporating the best of new and existing technology. There’s also a huge focus on quality; and all this must be achieved under tough public sector budget and time constraints.
Enhancing patient experience
Cancer facility designs should provide a sense of calm and reassurance, in a place where patients often feel frightened and overwhelmed.
Clear wayfinding, creating logical pathways and flows through the building are a key factor in order to reduce stress on patients, staff and visitors. Wayfinding and layout should also account for the fact that people often receive difficult news and information in these spaces.
Discreet, calming interview rooms are necessary, and some centres have private exit routes which avoid patients and families having to walk through a public waiting room after receiving bad news. In turn, waiting areas are evolving from serried rows of fixed seating to a more relaxed, hotel lobby-style layout, with chairs that can be moved around coffee tables or by windows.
Cancer treatments typically require patients to make multiple outpatient visits, and so designing simple pathways that enable visitors to create their own rituals – whether that means being able to go from a cafe out to a courtyard garden or terrace with a coffee, or into a quiet multi-faith space for contemplation – is important.
Giving patients a sense of autonomy and choice is vital and can lead to better healthcare outcomes. Most new cancer care centres with patient beds are now favouring single patient rooms. Evidence suggests inpatients will have a shorter length of stay if they’re in a single room, which provides a more peaceful environment, greater privacy, the ability to have relatives and friends sleep in their room, and also having loved ones able to help carry out their personal care. That said, some small, four-bed bays are still being designed into projects to provide patient choice.

Ensuring staff feel valued and supported
Providing care makes heavy demands on staff. There are currently more than 110,000 unfilled posts in the NHS, and staff retention is a critical issue for the service. Employees need to feel valued and cared for in their workspace.
These needs can be met in building design via good changing facilities, excellent provision for pedestrian, cycling and driving access and parking, restful facilities for breaks such as quiet rooms, sleep ‘pods’, spaces for indoor exercise such as yoga, and also private outdoor spaces to provide privacy and fresh air during shifts.
Access to education spaces should be seamless. Staff also require access to good education and training facilities, ideally close by or within the same building. Activity-based working involving a variety of workspace typologies is shifting from general workplace design into healthcare buildings. This is reflected in growing calls for these buildings to integrate, or at least have ready access to employee education, office space, clinical and support services such as Maggie’s or Macmillan support centres.
Creating adaptable buildings
Treating the shell and core as having a longer lifetime and the internal fitout as a shorter-term endeavour is a way of looking at buildings which NBBJ has been doing in conjunction with AECOM. Even if they are being procured as a single contract, designing the shell and core as distinct and separate from the internal fit-out configuration is being increasingly practiced. As cancer treatment and hospital design is changing and developing quickly, this approach enables faster changes and updates to the internal elements.
Standardisation – to have repeatable rooms where possible – provides benefits in terms of design, construction, maintenance, cost and clinical safety. As staff become more familiar with a room layout and equipment layout, it is much safer for them to be able to treat repeated patients without the added burden of understanding an unfamiliar space or layout. This also lends itself to Modern Methods of Construction (MMC).

Cancer care centres and net zero
Cancer care centres often have a higher energy usage (kWh/m²) than acute hospital facilities. This is due to a higher proportion of specialist radiotherapy and imaging equipment, usually within a smaller building footprint; the need to maintain a comfortable internal environment; and for specialist departments to incorporate a high fixed air change rate for infection control purposes. There is a potential conflict between NHS Net Zero Carbon (NZC) requirements, and the ability to offset the energy consumed by major medical equipment and Mechanical, Electrical and Public Health (MEP) plant serving energy intensive departments.
When developing net zero carbon energy strategies for cancer centres, it is important to ensure that actual energy usages are quantified during the early design stages. This should incorporate design solutions that allow clients to manage and benchmark their energy consumption, against design assumptions, so that they can achieve net zero once the building is in operation. At present, new-build healthcare projects target BREEAM Excellent as a minimum.
AECOM is designing solutions to enable new cancer centres to achieve net zero. Our approach includes designing all-electric facilities with a fabric-first focus, working with the architect to maximise the efficiency of the building through materials and components choices. Also central is the use of highly efficient decentralised air-handling plant to reduce both distribution energy losses, while maximising MMC.
Case study: Clatterbridge Cancer Centre
The Clatterbridge Cancer Centre in Liverpool is part of a cluster of world-leading specialist hospitals within Merseyside, including the Alder Hey Children’s Hospital and the Liverpool Heart and Chest Hospital.
The 11-storey, 110-bed NHS facility opened in June 2020. AECOM provided building services engineering, civil and structural engineering, acoustic engineering and sustainability as well as BREEAM and environmental services.
In collaboration with architect BDP, the focus from the outset was on designing a low energy building with a fabric first approach. A high-performance facade was integral to achieving this, as it insulates the building while maximising daylight penetration and thermal comfort for users.
Dynamic control systems help the building to perform over 50 per cent better than the Department of Health’s guideline carbon targets. More than 30 per cent of the building’s electrical demand is generated on site by low and zero carbon systems, including photovoltaic panels.
Modern methods of construction have been used wherever possible: 30 per cent of the structure comprised modular components. Prefabrication and modularisation of MEP systems in particular aided on-site construction and improved quality of build, cutting timescales and reducing on-site health and safety risks. The project is rated BREEAM Excellent.

Cost model: Cancer care centres
We have built a cost model for a new-build cancer centre adjacent to an existing hospital site. The facility has a gross internal floor area of 15,000m2 and is located in the South-east. The building aims for a BREEAM rating of Excellent and includes linear accelerator (LINAC) and laboratory testing space. Costs are based on Q2 2022 and include group one and fitting of group two furniture, fixtures, and equipment, concrete LINAC bunkers, and general labs.
You can download the cost model here.
This is an abridged version of an article that was first published in Building magazine. You can read the full article by clicking here.
The post A holistic approach to designing cancer care facilities appeared first on Without Limits.
]]>The post Imagining the future of healthcare delivery in 2070 appeared first on Without Limits.
]]>The coronavirus pandemic, technology advances and climate change are radically changing our approach to and reliance upon healthcare, which is increasingly informed by science-based evidence. Real estate is having to adapt, but what does the future really hold for healthcare delivery?
In our London 2070 report, which sets out our vision for the future city region, experts and thought leaders from across AECOM pooled their knowledge and aspirations. We imagined what a resilient, interconnected, responsible and balanced city region might look like in fifty years’ time. Healthcare delivery was an important part of that conversation.
In this first half of this article, we look at how current trends may shape health real estate strategies over the next five decades (listing action points), and in the second half we imagine what healthcare delivery and real estate might look like in a world where personalised and genetic-led preventative treatments have become the norm.
Where we are now and where we are going
Technology is constantly changing the working methodologies of doctors and surgeons. 3D imaging and laser technologies are facilitating less invasive, successful treatments while implantable medical devices can automatically monitor and regulate a raft of health conditions. Doctors can now work remotely and even perform robotic surgery.
The coronavirus pandemic caused a shift to remote diagnosis and treatments, and this will accelerate the development and adoption of technology-led healthcare as we move forward. There are many positives to this, though the challenges of how best to deliver local and personal patient care as well as targeting provision to reduce health inequalities will need to be addressed. We anticipate that this technology-led approach will lead to a rethink of health real estate strategies and will also stretch health and social care services to consider how and where healthcare is delivered, particularly as changing demographics will mean there are more older people to look after.
 Gradually, we expect that the cost of healthcare delivery from added demands of an aging population will be tempered by a preventative-led approach, informed by studies such as one published by the Journal of Epidemiology & Community Health (2017) which showed for every £1 invested in public health there is an average £14 saving in future healthcare costs. In the near future, wearable devices will transmit data from implants providing frontline care and advice in the home through AI-led algorithms. Secure data will be shared via the cloud to enable personalised genomic-led prevention and treatment to tackle the increasing prevalence of chronic conditions. The UK government has already set out its ambitions to create the most advanced genomic healthcare system in the world by 2030[1] which will be stimulated by the work underway in the innovative economic clusters across city regions and their health, research and university clusters.
Gradually, we expect that the cost of healthcare delivery from added demands of an aging population will be tempered by a preventative-led approach, informed by studies such as one published by the Journal of Epidemiology & Community Health (2017) which showed for every £1 invested in public health there is an average £14 saving in future healthcare costs. In the near future, wearable devices will transmit data from implants providing frontline care and advice in the home through AI-led algorithms. Secure data will be shared via the cloud to enable personalised genomic-led prevention and treatment to tackle the increasing prevalence of chronic conditions. The UK government has already set out its ambitions to create the most advanced genomic healthcare system in the world by 2030[1] which will be stimulated by the work underway in the innovative economic clusters across city regions and their health, research and university clusters.
Successive digital strategies[2] to join up health and care data, along with the Centre for Digital Built Britain (National Digital Twin Programme) proposals such as the one for London’s Healthcare Infrastructure (LHI), are already informing the OneLondon digital approach, which aims to ensure clinicians across the capital have access to patient information at the point of care. This is being adopted in other city regions, and nationally.
But the move to a future healthcare approach is not solely about treating physical health. Increasing the use of technology and automation must not sacrifice healthcare’s important role in supporting individual and community wellbeing or the resilience of public health services, including the ability to tackle future pandemics through local action.
Consequently, we also anticipate a renewed focus on mental health, accompanied by a workstyle evolution, as flexible working and a reduced-hours working week become the norm. In Japan, Microsoft has seen a 40 per cent increase in productivity after switching to a four-day working week, while Sweden and Finland are planning similar moves. Cutting the working week could enhance wellbeing and free up more time for self-development and community-centred activities such as volunteering, mentoring and providing extended social care – all part of rebalancing our lives with a greater focus on civic purpose and shared community responsibility.
Heathcare delivery in 2070
 By 2070 the innovations and application of technologies developed in the health-tech clusters of the city and region will have had a profound effect on the delivery of healthcare services. With widespread adoption of genomic-led treatments that lessen the day-to-day demands on the system, healthcare real estate, as we know it, shrinks as delivery is liberated from place-specific constraints. Instead, the focus evolves into person-centric, preventative care supported by secure data sharing through the region’s highly-developed digital connectivity.
By 2070 the innovations and application of technologies developed in the health-tech clusters of the city and region will have had a profound effect on the delivery of healthcare services. With widespread adoption of genomic-led treatments that lessen the day-to-day demands on the system, healthcare real estate, as we know it, shrinks as delivery is liberated from place-specific constraints. Instead, the focus evolves into person-centric, preventative care supported by secure data sharing through the region’s highly-developed digital connectivity.
The early elimination of diseases will mean that people simply will not need to interact with the system as much as they once did, most notably in the types of facilities that deliver reactive acute care, such as hospitals.
Underpinning this model of care, the healthcare system will be organised around health management in the home. In the medium to long term, telemedicine will be the norm, with diagnostics and examination coming to the patient rather than the reverse. Low cost drones will securely distribute medication and in-home diagnostic equipment will allow community healthcare professionals to focus on personal care and engagement.
Health management in the home will be supported by a network of connected smart ‘hives’, so-called because they take inspiration from the community and support offered by beehives. These “hives” will serve a number of functions related to the ongoing survival of the colony and the success of the hive is entirely dependent on the coordinated actions of individuals working together. In a similar way, healthcare hives will draw together healthcare professionals and community volunteers to meet local needs. In 2070, our integrated care system will comprise community-based Health and Wellbeing Hives (H&W Hives) and regional Medi-Hives, centres of excellence for acute and chronic conditions,
-

Community-based H&W Hives will be at the heart of personalised delivery when light-touch, generic patient intervention is required With the majority of primary healthcare delivered in the home, community-based H&W Hives will be at the heart of personalised delivery when light-touch, generic patient intervention is required, dealing with all non-emergency acute care, also providing mindfulness, self-care advice and mental health treatment.
Located in ‘civic hubs’ in repurposed buildings on local high streets, the H&W Hives will be highly valued by the communities that they serve. For many, the H&W Hives will be a short walk away or easily accessible by autonomous pods. The H&W Hives will be further supported by diagnostics vehicles carrying compact technical equipment which will be able to make hyper-local journeys within local communities. By 2070, understanding around early years development in relation to wellbeing and mental health will be well-developed[3]. People suffering mental health issues will receive preventative care early and further support in the community, with acute centres for those who need them. For the elderly and vulnerable, the H&W Hives will also provide the essential human connection that will address isolation to balance technology-led care.
- Medi-Hives will be regional centres of excellence. Combining white and dark space, the Medi-Hives will house specialist science, treatment and manufacturing facilities, undertaking the growth and regeneration of nerves, limbs and organs. They will also offer personalised and regenerative medicine based around a patient’s genome, act as trauma centres and support the coordinated response to future pandemics. For those in need of greater support and treatments, flying ambulances will extend their reach.
Significantly, both the H&W and Medi-Hives will play a vital role in improving the quality of life of the UK’s thriving population of centenarians enabling them to play an active part in UK culture and economy.
Recommended next steps to create future-ready healthcare delivery
The post Imagining the future of healthcare delivery in 2070 appeared first on Without Limits.
]]>The post Designing for primary care change in Northern Ireland appeared first on Without Limits.
]]>In 2016, a report chaired by Professor Rafael Bengoa found that the current model of health and social care provision in Northern Ireland was financially unsustainable and unable to meet the needs arising from demographic change, increasing demand, health inequalities and a disempowered workforce.
The ‘Systems, Not Structures: Changing Health and Social Care’ report noted that “the trends in healthcare towards a more personalised, preventative, participative, and predictive model of care will not happen at the necessary speed in the present fragmented and reactive model of care,” describing the current situation as a “burning platform.” In a 2019 update on the report, Professor Bengoa stated that the pace of change had clearly increased but more was required.
Then in 2020, coronavirus hit and accelerated changes to the primary care landscape, transforming almost overnight the way consultations were held. Only a small percentage of GP consultations were undertaken by phone or video conference prior to the pandemic, yet at the peak around 70 per cent of all consultations were virtual.
Combined, these factors have stimulated an essential rethink of how primary care facilities are designed. Healthcare architects now have to deliver contemporary facilities that meet patient, clinical and operational needs while providing therapeutic and inspiring environments that enhance the wellbeing of all users. Facilities must also serve their communities both in and out of working hours and must be flexible enough to meet future demand and change.

This article highlights five areas that our specialist healthcare architects and cost managers focus on when designing sustainable health and wellbeing centres, drawing upon best practice learnt from delivering award-winning contemporary facilities across the UK and the island of Ireland.
1/Comprehensive stakeholder engagement
What does comprehensive stakeholder engagement on a healthcare facility look like in Northern Ireland?
Firstly, it is important to establish strong relationship with all parties right at the start of any given project, which in the case of Northern Ireland includes the Health and Social Care Board, Local Commissioning Groups, patients, staff, design consultants, local authorities and local community groups.
Secondly, the focus should always be on proactive, timely and professional interaction, engaging with the right people at the right time throughout the design and delivery of the project, with fair consideration given to all viewpoints. Both a formal and informal approach to stakeholder engagement is important, depending on the objectives and always with an aim to facilitate a full understanding of each other’s needs and aspirations. On our recently-delivered Goodman’s Fields Medical Centre in London for example, we incorporated Bengali translations into the signage to be inclusive of the high percentage of Bangladeshi patients as identified through extensive community consultation.
Thirdly, it is important to appreciate that all stakeholders are experts in their areas and that listening and learning from their experience and knowledge is a vital ingredient for success.
2/Design that’s flexible and adaptable
Future change to primary care is inevitable – some changes we can predict, others remain unknown. It is important therefore that adaptability and flexibility are built into the project brief as essential requirements.
As primary care service providers adapt to meet new trends and demands so must the buildings they occupy. We are seeing a shift towards larger buildings with flexible and interactive spaces that can be repurposed quickly. Our healthcare architects are designing and delivering health centres that will be used as a community meeting space out of hours. However, if there is an immediate need for evening appointments these spaces can be freed up for treatment.
The best way to meet this need is to keep the architectural, structural and services design simple. Over-specification, over-complication and a design based on short-lived, quick fix technologies should be avoided. It is easier to adapt spaces to alternative uses if room sizes and dimensions are standardised and sit within floor plans that are designed to a planning grid. Likewise, we design services with appropriate overcapacity as well as making sure that plant and service access spaces can accommodate future building service expansions, adaptation or replacement.
3/Creating positive and therapeutic environments
Ultimately, healthcare environments should stimulate and support the power of interpersonal relationships between patients, families, clinicians and staff to transform experiences and improve health and wellbeing outcomes.
The ideal way to design environments that promote wellbeing, privacy and dignity is through a collaborative and research-based approach. Every aspect of the design must be carefully considered with special emphasis given to natural light, welcoming entrances, reception and waiting areas and ensuring staff have good observation points. Natural, warm and soft palettes of colours work best alongside materials with good acoustic properties to create comfortable environments for patients and staff. As part of our interior strategy, and in collaboration with clients, we select healthcare-appropriate furniture which is complementary to the overall look and feel whilst ensuring it meets infection control requirements. The combined results are far removed from the perception of hard chairs and bare walls that many associate with visiting the doctor.
Lighting is also important. Our architects work with in-house lighting designers and engineers to ensure the ambient lighting provides areas with overall levels of brightness, illumination and the right colour temperature. It is important to provide examination lighting within each clinical room to allow clinicians to examine or treat patients appropriately.
Furthermore, as primary care centres increase in size, they can become more challenging for patients to navigate so aligning the patient journey with key architectural and interior elements is central to alleviate excessive signage.

4/Sustainability
Sustainability is a key driver of change in the design and costing of primary care facilities. As environmental scrutiny is heightened throughout the world, healthcare providers are focused on reducing their carbon footprint. The sustainable design standards that were once considered as ‘nice to haves’ are now a given, and new and refurbished buildings must achieve a high sustainability rating. Through early definition and analysis of the likely embodied and operational carbon of a building, renewable energy and an offset approach is factored into the design of our primary care buildings.
Important elements include maximising natural daylight and ventilation, the use of efficient lighting, heating, mechanical ventilation, and air conditioning, as well as the specification of the most appropriate insulation and low energy IT and appliances. With new build projects, our default approach is to use renewable energy sources such as photovoltaics, ground-source or air-source heat pumps, rainwater collection and high-performance building envelopes.
5/ Delivering design principles to budget
There are several factors that can influence the costs of developing a new healthcare centre. Specific location and site conditions will automatically influence development costs but there are also other factors which will influence the design and hence cost of individual centres.
With the current focus on digital consultations, there will be a greater emphasis on resilient and quality IT installations. Equally the need for improved ventilation, highlighted by the pandemic, will increase the loadings on plant and associated costs. Over the longer term however, the drive towards zero carbon is also expected to increase the capital cost of developing new projects across the construction sector and primary healthcare centres will be no exception.
Conclusion
Primary care is no longer about reacting to symptoms and illness. Primary care clinical services are evolving quickly to include health and wellbeing, delivered directly to communities. As services and staffing are decentralised from within acute hospitals, it is crucial that the next generation of primary care centres are able to flex to support current – and future – clinical and digital strategies. They will need to be positioned at the heart of the communities that they serve, with adaptable spaces to support the delivery of new models of care.
Healthcare centre cost model

Our cost model is for the development of a typical healthcare centre (gross floor area = 1,550m2) to be used by GPs, community nurses, midwifery services, mental health services, social services and support services based in Northern Ireland. The development is based on achieving a BREEAM Rating of Very Good. The model assumes a single / part two-storey development.
Costs are based on Q3 2021 and include for Supply and Fix of Group 1 and Fixing of Group 2 items and an allowance has been included for external works. The costs exclude utilities, contingencies, professional fees, surveys and VAT.
In addition, costs reflect a single stage competitive tender with a standard construction contract. The rates would need to be adjusted to account for actual specifications proposed, specific location / site conditions, procurement route and programme.
The post Designing for primary care change in Northern Ireland appeared first on Without Limits.
]]>The post Embracing innovation to transform mental healthcare facilities appeared first on Without Limits.
]]>We are witnessing a revolution in the way mental healthcare provision is delivered across the island of Ireland. New holistic care models, based around central tenets of therapy and recovery rather than isolation and institutionalisation, are informing the design and location of pioneering new facilities,

helping to destigmatise mental health.
Increasingly, innovative design methods are underpinning the delivery of these new secondary care facilities, where digital tools are leveraged to create award-winning environments that are both inclusive and nurturing, yet robust enough to ensure the safety of both patients and staff – a delicate balance to strike.
This article draws on our experience of delivering some of these new healthcare facilities – from acute services to forensic mental care and children’s support units – to demonstrate how a digital-led approach can improve delivery, increase operational effectiveness and support the person-centred care model being rolled out across the island of Ireland.
The enormous costs of poor mental health
More than one in six people in EU countries (17.3 per cent) have a mental health problem in any given year – the figures for the island of Ireland show a marginally higher percentage (18.5 per cent).
Coronavirus has added a further twist. Isolation and lack of access to formal and informal support during extended lockdown periods have been devastating for those with existing mental health issues, with some evidence from the UK pointing to an 8 per cent increase in cases as a direct result of the pandemic.
Aside from the significant human and social costs (through reduction in quality of life, depression and pain etc.), the wider economic costs are enormous – up to as much as four per cent of GDP across EU countries, or over €600 billion. In the Republic of Ireland, estimates suggest that costs amounted to 3.2 per cent of GDP in 2018.
Recommendations set out in reviews by the National Health Service (NHS)[4] and Health Service Executive (HSE)[5] have paved the way for a radical step change in the way mental health care provision is delivered to try and minimise these costs.
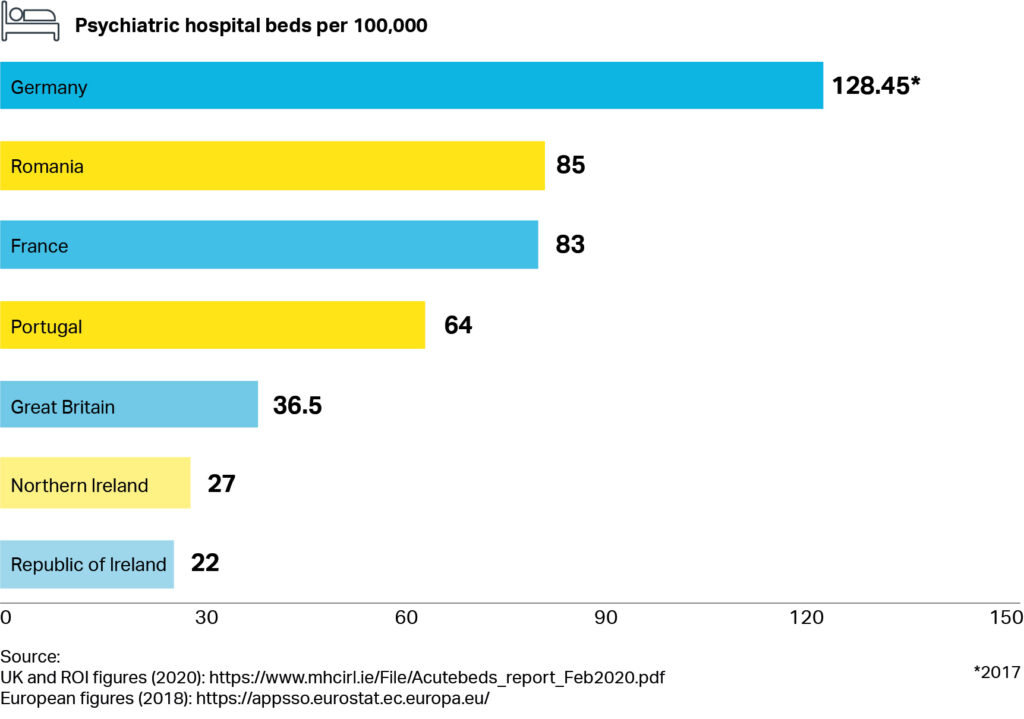
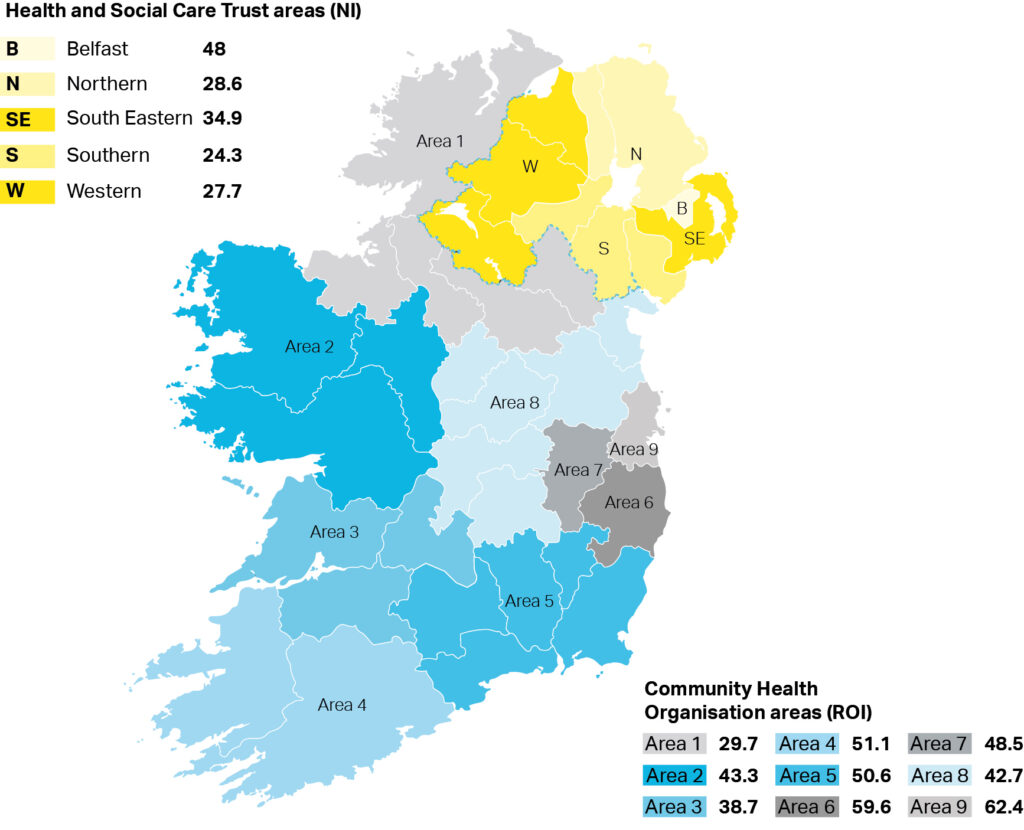
While there has been a steady if modest increase in overall gross non-capita mental health budgets in recent years, the current percentage allocation to mental health still falls short of recommended levels – and the number of beds per 100,000 across the island of Ireland is low in comparison to other EU countries (Figure 1). Demand for services is still acute, particularly in urban areas across the country (Figure 2).
New best practice is emerging
Changes in the delivery of mental health care provision have clear implications for how healthcare trusts manage, design and deliver their estates: this is where good design and technology step in.
Risk assessment is a good example. Risk assessment processes are an intrinsic part of mental health. Creating a secure environment for patients and staff is a critical requirement particularly in acute units – where patients can become distressed, disruptive and destructive with potential for self-harm, violence and even loss of life.
In the new intensive support unit for children in Glenmona in Belfast, where we needed to make the facilities as inclusive and homely as possible, we took a risk-based assessment approach to reduce the safety requirements while using cutting-edge design to ensure compliancy. In low and medium risk areas the proposed interior design means that safety and anti-ligature features can be more discretely placed, and design layouts promote line of sight limiting the amount of surface protection measures.

We took a similar approach at the Acute Mental Health Inpatient Centre – a recently-opened state-of-the-art facility located in Belfast City Hospital. There, technology has been leveraged to minimise at risk situations for both patients and staff. Isolation controls can identify water misuse allowing staff to immediately shut off supply to patient rooms. Smart electrical design removes self-harm electrocution risk.
Innovations around personal technology and sensors – applications of which continue to advance –complement the safety measures embedded within the physical building. At the Inpatient Centre in Belfast for example, radio-frequency identification (RFID) is integrated with the alarm systems enabling real-time patient and staff tracking. In case of emergency, immediate staff-assist and staff-attack response location information is communicated to site-wide display stations.
Costing benefits
Costing the benefits of these systems needs to happen early. A socioeconomic cost benefit analysis is the best way to measure the impact of an improved environment and the reduced risk to staff and patients. Generally, the more area within the building, the greater the capital cost. However, designing solely to Health Building Note (HBN) guidance can potentially impact on the therapeutic environment within mental health facilities. Careful consideration must be given to incorporating daylighting, natural ventilation and single-loaded corridors which provide good levels of natural light and views out to external spaces.
There are both positive and negative revenue and operational impacts of deviating from HBN guidance. This was demonstrated by a mental health trust who decided to increase all its bedrooms with en-suites from 15m2 (as per HBN guidance) to 23.5m2. This enabled the trust to admit patients of all levels of mobility, resulting in never having to turn away a patient who required a larger room. This decision resulted in the trust achieving the optimum 85 per cent occupancy rate which, in turn, had a positive revenue impact.
Conversely, if trusts choose to deviate from HBN guidance and drive areas too low, it can result in a smaller facility, with the same quantity of rooms, albeit smaller, and similar staffing level requirements. Smaller rooms can prevent disabled or obese patients from accessing the facility which can reduce the potential revenue that could be gained from a more flexible design approach.
The benefits of digital delivery
The best way to incorporate these enhancements is to design buildings digitally.
This is happening in Scotland where we are working with Health Facilities Scotland (HFS) and NHSScotland (NHSS) to deliver on the Scottish Government’s Digital Health and Care Strategy. The first step was to embed Building Information Modelling (BIM), which allowed NHSS to then create a digital estates strategy. One of the key components of this is the digital twin — a shift from a deterministic to a more probabilistic, dynamic model.
Via digital twinning, NHSS aims to link its physical assets (buildings and potentially end-users) to a digital representation, using data from sensors and analysing variables such as condition, efficiency and real-time status. This connectivity coupled with data analytics will reform facilities’ levels of operational effectiveness, generate extra insights from the digital twin to help reshape and improve services, and support person-centred care.
Using data to achieve parity of esteem for mental health
These facilities are at the vanguard of mental health care across the island of Ireland. Cutting edge design and technology is already improving the quality of patient care, and better protecting staff. Likewise, digital tools and processes are delivering the next generation of facilities efficiently, achieving value for money.
It is important that this momentum is not lost. Collating data and user experience evidence is the next step. In combination with in-depth cost model knowledge, a strong case can be made for further investment, and another step can be taken along the road to achieving parity of esteem for mental health.
The post Embracing innovation to transform mental healthcare facilities appeared first on Without Limits.
]]>The post Net zero heroes: helping the NHS achieve its carbon reduction goals appeared first on Without Limits.
]]>The much anticipated publication in October of the NHS Delivering a ‘Net Zero’ National Health Service comes as the NHS embarks on a long-term programme of investment in health infrastructure. With £3.7 billon funding to build 40 new hospitals, delivering on the net zero commitment is going to require a new approach.
Net zero means reducing the carbon emissions associated with a building’s usage and construction to zero or below. Thanks to the huge and varied demands required of them, hospitals have a large carbon footprint from both construction and operation, although modern design and a decarbonised grid look set to radically reduce operational emissions in future. To achieve the NHS objective, hospital trusts should look closely at the building structure, which our analysis shows has the potential to be most impactful when it comes to reducing embodied carbon demands.
As NHS Chief Executive Simon Stevens makes clear, the climate emergency is also a health emergency. Leading by example, the NHS – which is responsible for around 4 percent of the nation’s carbon emissions – has set out a clear objective of reaching carbon neutrality by 2040.
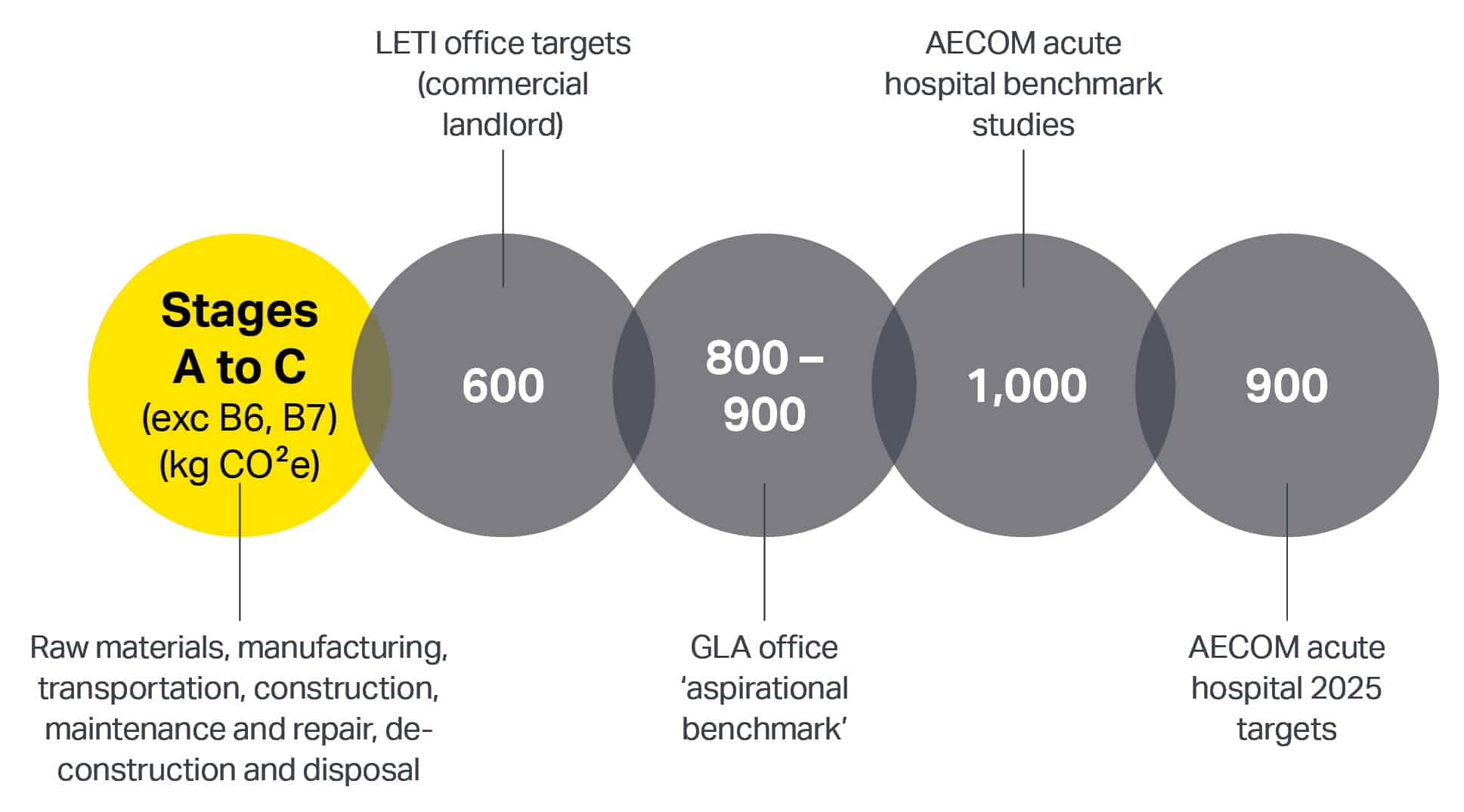
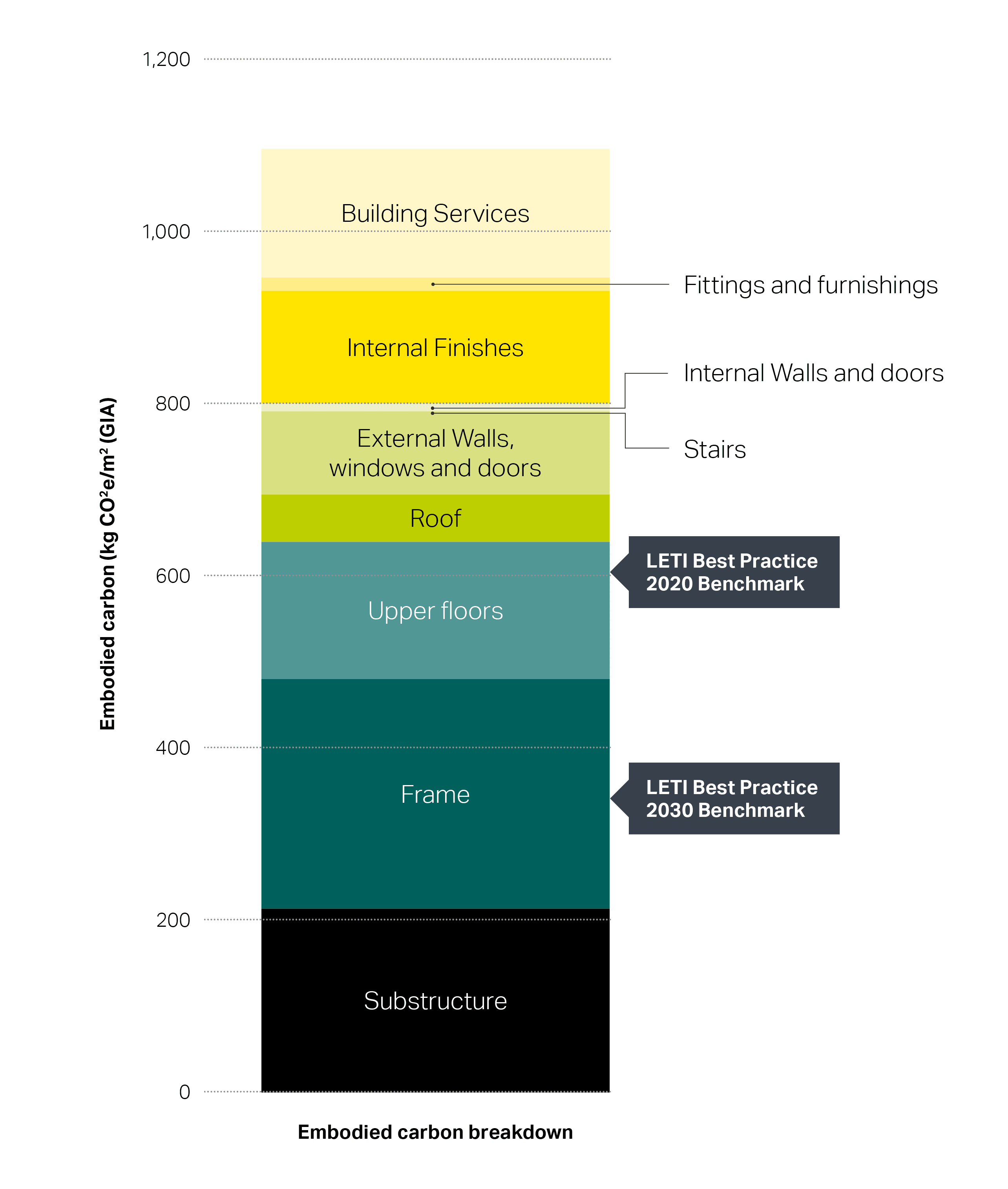
Official targets for embodied carbon have not yet been set for new hospitals, but we have compiled what we think those targets might look like by using targets for Greater London Authority office buildings, those put forward by the London Energy Transformation Initiative, combined with AECOM benchmark studies of both office buildings and recent completed hospitals. Figure 1 demonstrates the range of ‘do minimum’ and ‘aspirational’ targets for both GLA and AECOM benchmark studies. This has enabled us to set our own targets as shown.
To inform net zero strategies, the UK Green Building Council and LETI have compiled a set of building guidelines, to which AECOM has contributed. In addition to these considerations, hospitals have specific requirements that deserve careful consideration.
On an individual scale, hospitals contain a variety of departments ranging from administration through to theatres and imaging. Each space has different structural design requirements which need to be addressed: from space requirements influencing grid spacing, to floor loading requirements and vibration limits. The buildings also need to accommodate complex equipment and mechanical, electrical and public health (MEP) routing requirements, with high space demands for services. Medical equipment such as MRI scanners are heavy and have stringent vibration criteria.
To address the specific and changing nature of healthcare provision, hospitals require adaptable and flexible solutions – as the rapid re-purposing of spaces during the coronavirus crisis highlighted. In the future, hospital buildings and facilities must be designed to respond to multiple and fast changing health situations, with space for new technologies.
From operational energy efficiency to the question of whether to build new or refurbish, there are many considerations for hospital trusts to consider. In this article, we are going to focus on what our own analysis has shown to have the most impact on reducing embodied carbon emissions: the building structure.
Thanks to experience delivering carbon efficient buildings such the GSK Carbon Neutral Laboratories for Sustainable Chemistry, the world’s first carbon neutral lab, and the LEED Platinum facility at NASA Ames Research Center in California, AECOM has been building up a library of carbon data relating to a building’s structure. Figure 2 shows that half of the embodied carbon of a typical office building is due to the structure. When it comes to hospitals, the percentages are similar, despite the unique challenges placed on such buildings.
Three considerations for net zero hospital design
To reduce the carbon footprint of a building structure, three considerations are key: design, materials choice and offsite manufacture and assembly.
1/ Design
Three broad principles will help achieve the best energy efficient outcomes from design:
a) A pragmatic approach
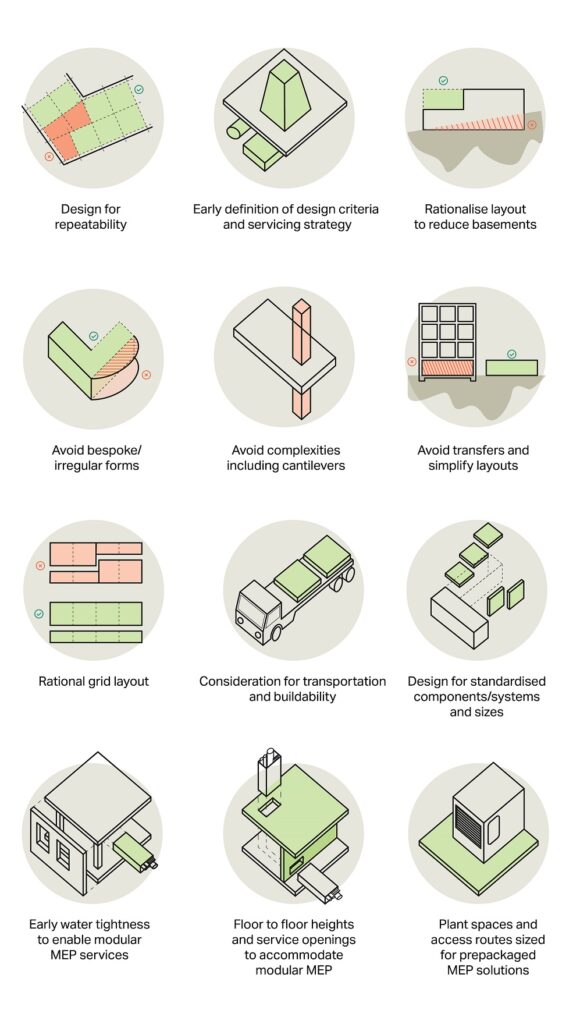
To rationalise material use and reduce carbon content throughout the building, the following lean engineering practices will help:
- providing regular grids,
- maximising the repeatability of structural elements,
- designing to standard component size as much as possible,
- maximising pre-fabrication potential,
- limiting the structural spans,
- avoiding irregular shapes and structural complexities such as transfers.
Reducing the use of basements can also have significant savings. AECOM benchmark studies have shown that 20 per cent of embodied carbon can be found within the substructure. This figure rises exponentially with the inclusion of basements.
b) Avoid over-specification
Like the human body, the different elements of a building are inter-connected, and prescribing a specific outcome for one variable can put pressure on other variables. The key is achieving a balance between flexibility requirements, which require additional functionality, and efficient design. This requires input from NHS estate managers, clinical planners and the design team as a whole to first establish flexible criteria and the strategies to implement these.
c) Applying circular economy principles
Design focused on eliminating waste and re-using resources can increase building life span as well as incorporating flexible structural arrangements. From the outset, consideration should be given to what happens at the end of a building’s life, designing for dismantle and re-use.
2/ Materials choice
The choice of materials used in construction has the potential to impact embodied carbon significantly, and exploring the most appropriate material should be considered from the outset. As Figure 3 shows, using sustainable materials such as timber, and reducing high carbon content materials such as swapping cement with replacement materials can make a huge impact.
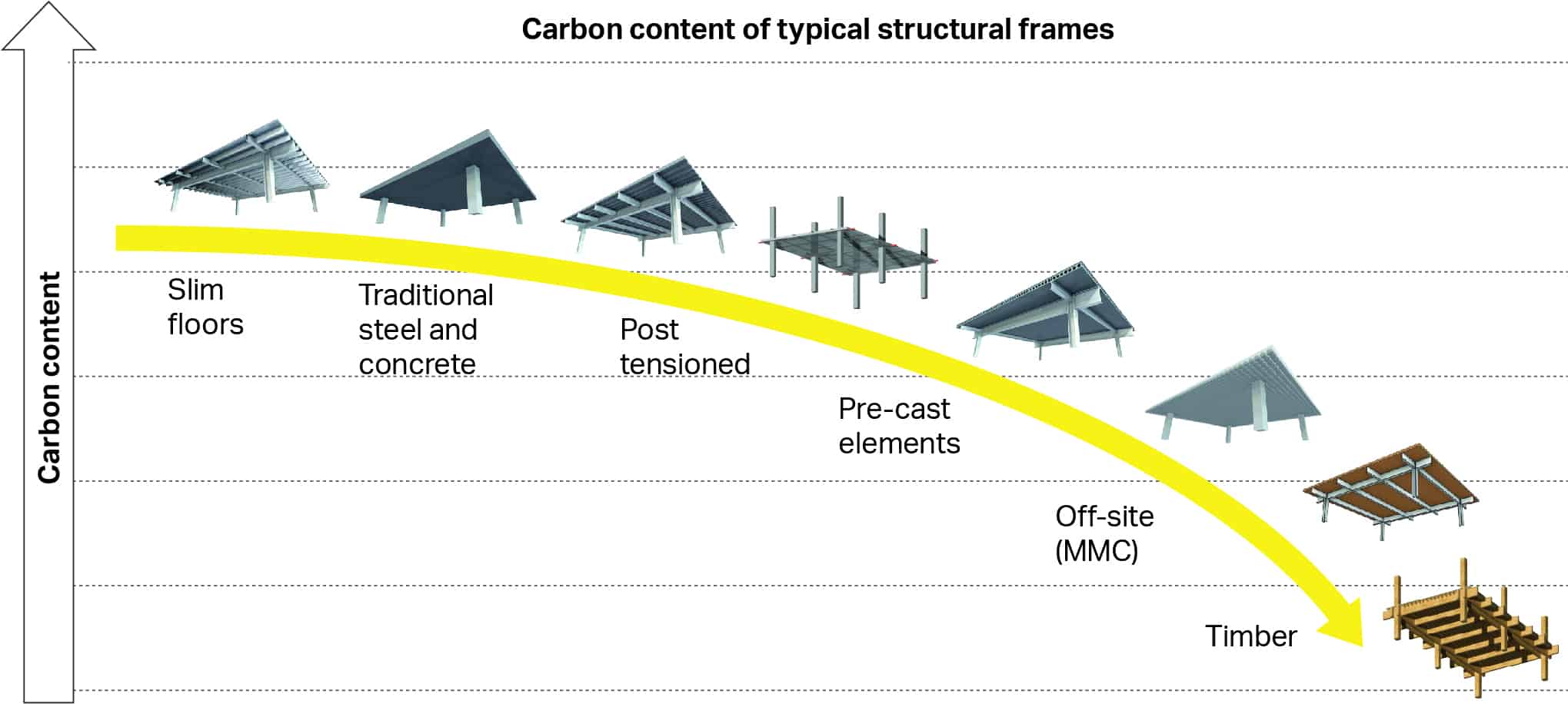
Developing designs around the chosen material will maximise carbon savings. AECOM has developed bespoke tools to define materials choice by enabling rapid prototyping of early stage options and reporting against performance criteria including carbon content. Along with our carbon calculators and advanced analysis tools we can then maximise carbon savings throughout the design development of the building.
A timber hospital?
The standalone winner in terms of carbon content is timber, which could even be carbon negative. However, following the Grenfell Tower fire tragedy in 2017, the government banned the use of structural timber along with other combustible materials in external walls of buildings over 18 metres. The ban has had wider implications on the desire to adopt structural timber and insurance difficulties. This shouldn’t preclude timber as a viable structural frame option for hospitals, but while nervousness remains regarding its use in the whole structure, consideration should be given to ancillary structures or selected structural elements.
3/ Design for offsite manufacture (Modern Methods of Construction/MMC)
To support the modernisation of the construction sector, off-site production is being actively encouraged by the government, whose five central departments have adopted a ‘presumption in favour of offsite construction’ for public buildings. The NHS looks to be following suit with a requirement to explain how , when applying for funding from government.
Through efficient energy usage in manufacturing techniques and the reduction in material usage and waste, offsite production. Evidence collected so far suggests that construction waste and site CO2 emissions can be more than halved through a DfMA approach compared with traditional practices. It can take many forms, from constructing individual structural elements (steel, concrete or timber) through to full building modules. Taking full advantage of these benefits requires structural engineers to adopt the design principles stated above from the outset.
The world’s first ‘net zero’ national health service
With NHS net zero carbon hospital standards due to be set in Spring 2021, the business case for the planned new hospitals will need to demonstrate the energy strategies to meet them. The challenge is to not only meet these emerging requirements, but to pre-empt them. To be sustainable, the new projects should be built to serve current and future generations.
Tools and processes to deliver on these aspirations include rapid prototyping and optimisation software used from inception, through to advanced bespoke carbon calculators giving BIM linked real time carbon assessments through the detailed design phases. The planned 40 hospitals should be net zero heroes, carbon exemplars that set the trend for future NHS buildings and infrastructure.
The post Net zero heroes: helping the NHS achieve its carbon reduction goals appeared first on Without Limits.
]]>The post Integrated planning: why medical schools need a joined-up approach appeared first on Without Limits.
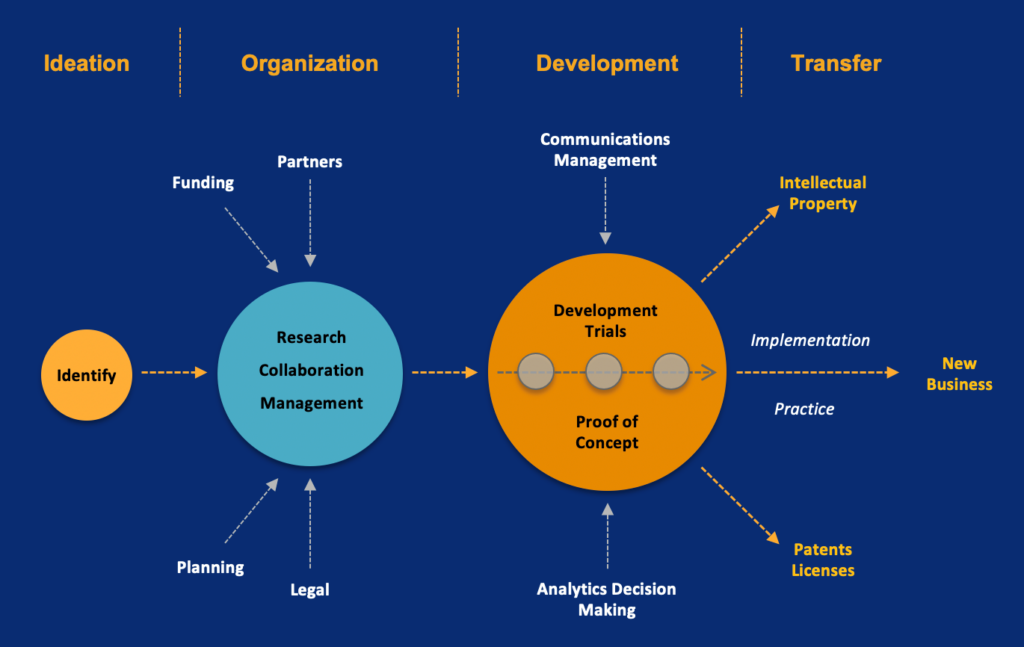
]]>Emerging from the pandemic, the medical schools that leverage lessons learned from operating at an unimaginable pace and with so much resilience and creativity will be the ones to lead the field. The question they should be asking is, “how do we build these new behaviors and processes into our organization so that we continuously raise standards in education and research in the years ahead?” The answer is integrated strategy.
In the past, planning was siloed with aspects of research, learning, business, operations and facilities addressed separately. In contrast, planning of the future will be integrated – embracing joined up thinking, increased collaboration and data-driven decision making.
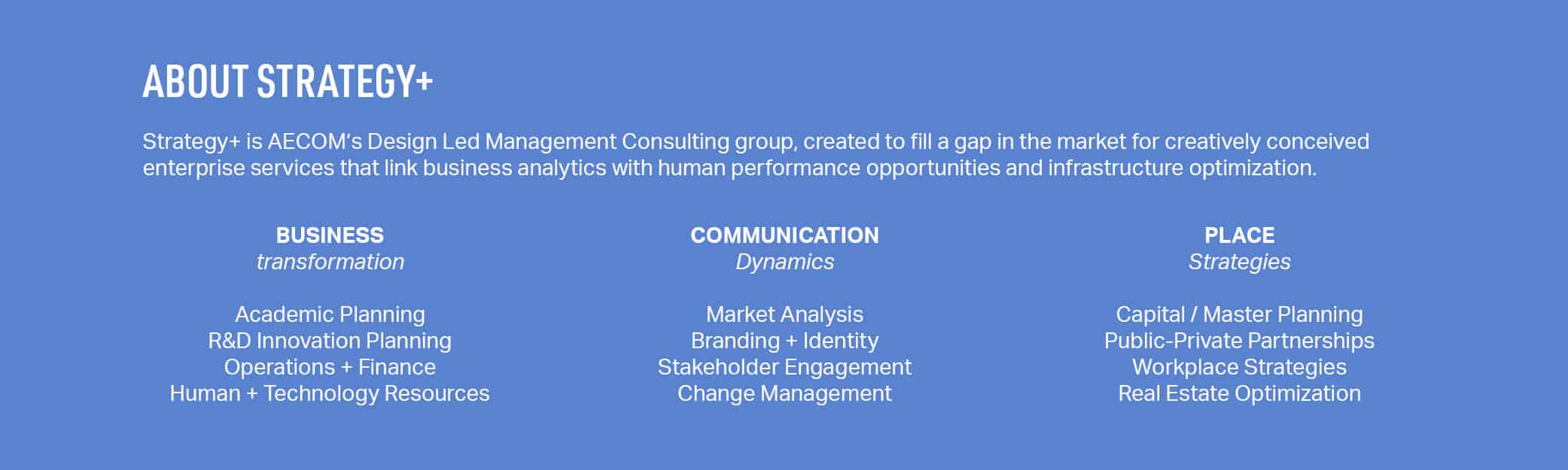
In this article, we identify six important aspects that are driving transformative initiatives in academic medicine. Even in the midst of the pandemic there are schools across the United States that are already reimagining their future by addressing these core themes. Strategy+, AECOM’s design-led management consulting studio has been working with these institutions to implement these approaches, and we include some of these case studies below.
 1/SYNCHRONIZED
1/SYNCHRONIZED
By aligning streamlined processes and policies, innovative activities, inclusive governance structures, new partnerships and service models with optimized resource allocation we can more effectively target the delivery of innovative real estate. To do this however, organizations need to move away from traditional siloed approaches where the focus tends to be on individual projects or processes. In contrast, taking a synchronized approach means aligning shared learning, research and administrative resources for greater efficiency. Using an inclusive governance structure, planning and communication can be synchronized. Organizational improvement can dramatically reduce change the need for space.
CASE STUDY: Lehigh University’s New College of Health engaged Strategy+ to design and implement a shared services model that leverages a ”concierge” capability. Cross-trained professionals are allocated a faculty group and provide personal-focused assistance in aspects of HR, student support, research pre- and post-award support, tech transfer and marketing.
 2/DYNAMIC
2/DYNAMIC
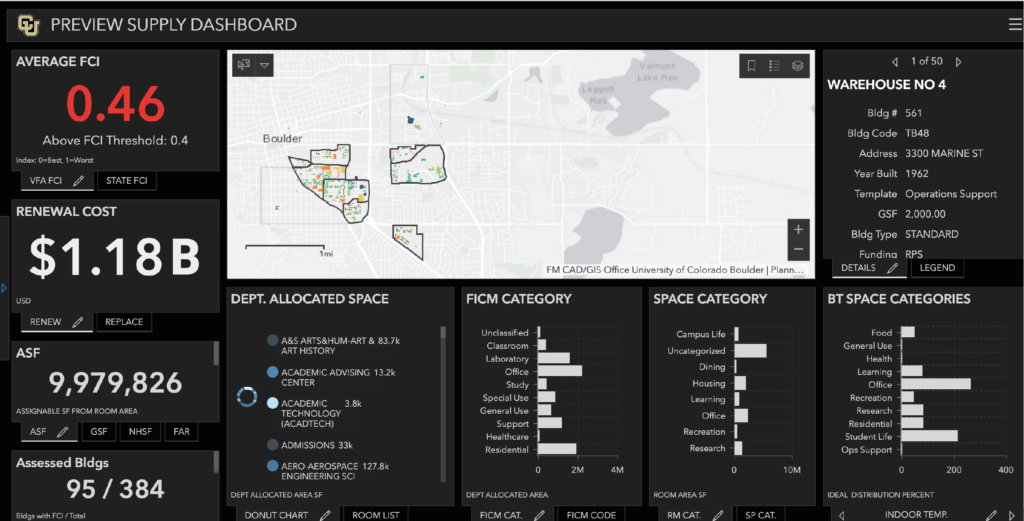
Taking a dynamic approach means leveraging mission-driven live analytic dashboards to make informed decisions on enrollment, research performance and future capital investments, rather than taking a static, non-data-driven approach that represents just one point in time. Interactive planning tools driven by live databases allows us to undertake real time modelling of changes in enrollment, pedagogy, new programs and research expenditures, and see the effect on financial, physical, human and technological resources.
CASE STUDY: University of Colorado, Boulder has engaged Strategy+ to create an interactive GIS academic planning tool. It facilitates the analysis of enrollment, revenue and costs, human resources, facility suitability, space utilization, new pedagogies, operating costs, and income generation to assess real estate solutions capacity to address evolving learning and research opportunities.
 3/DIGITAL
3/DIGITAL
The global pandemic has forced new learning, working, research and clinical practices to become mainstream and in response institutions are learning to look beyond their physical infrastructure. Moving forward, institutions must learn to leverage agile mobile working practices, and continuously adopt new technology and update curriculums to improve accessibility, efficiency and quality of multi-modal learning. For example, first- and second-year students have focused on virtual anatomy and interacting with standardized patients on-line. Third and fourth years learn on-line in redesigned clerkships involving faculty-guided, didactics and patient videoconferences. Digital infrastructure has increased faculty and staff mobility who can now work anywhere.
CASE STUDY: The University of California’s Riverside School of Medicine engaged Strategy+ to integrate collaborative digital experiences into its future education facility. For clinical skills we realigned contact hours for small groups in virtual anatomy, virtual standardized patients and i-human encounters. We also realigned its workplace strategy to integrate mobile teaching and administration.
 4/MISSION-DRIVEN
4/MISSION-DRIVEN
Colleges of medicine are increasingly using mission-focused strategic initiatives and metrics-driven goals to define their brand and focus their academic vision. Mission-driven planning develops these academic, financial, operational and experiential differentiators into a timeline of metrics-based targets that drive the types and extent of optimal research and learning facilities. This marks a shift away from traditional planning-driven approaches that focus on development sites and their phased delivery.
CASE STUDY: NYIT College of Osteopathic Medicine asked Strategy+ to develop research and technology transfer focus areas as part of its strategic plan. Leveraging its strengths in anatomy, esports and comprehensive whole person practice they will concentrate on recruiting osteopathic research specialists and grow targeted research income.
 5/TRANSFORMATIVE
5/TRANSFORMATIVE
The pandemic has emphasized the need to reassess traditional programs, curriculum and student support delivery modalities. New approaches to the social determinants of health, public health, population health and telemedicine are driving new forms of inter-professional teaming. This is in contrast to traditional approaches where consultation and collaboration occurs solely within the organization.
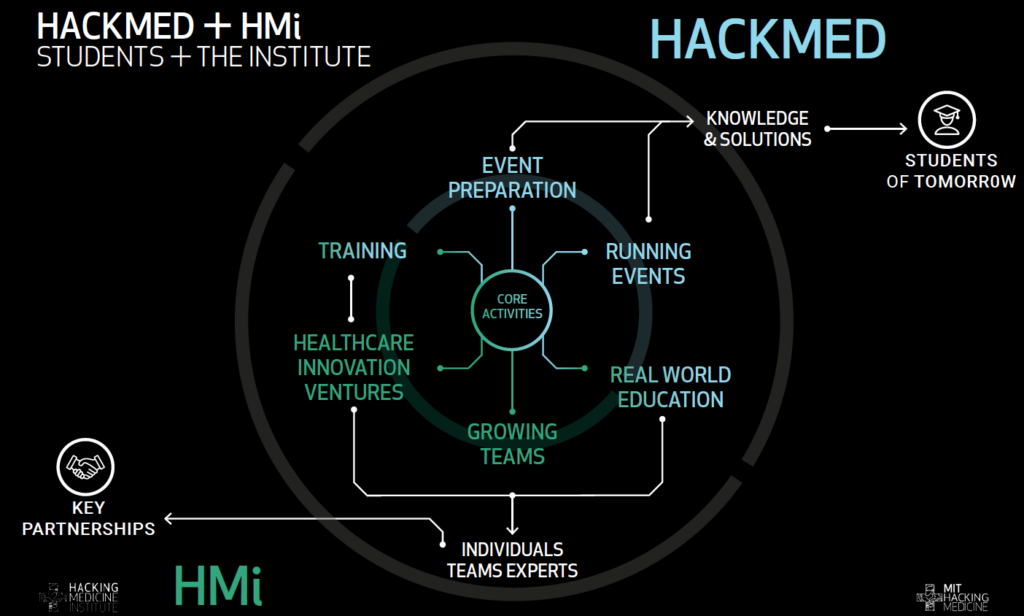
CASE STUDY: MIT Hacking Medicine Institute (HMi) As a dramatic departure from how MIT currently leverages its work into outcomes and impact, HMi’s vision, virtual operational model, governance structure and funding strategy is intended to disrupt the health industry by crowdsourcing targeted health related challenges and accelerating solutions to market.
 6/OUTCOME-BASED
6/OUTCOME-BASED
It’s not enough to just take an aspirational approach. Goals must have targets. Equate your initiatives and facility decisions with metrics for equity, diversity, inclusion, economic mobility, workforce needs and community impact. Medical schools are employers – they support populations and undertake research activity that has major economic and social impact. Outcomes-based planning focuses not only the implications that investment decisions have on facilities and infrastructure, but also on regional economics, workforce needs and livability.
CASE STUDY: University of Texas Rio Grande Valley Medical School (UTRGV) required a roadmap for regional education, health and economic development. Their plan directly relates the provision of cost-effective medical education, the creation of industry-focused R&D clusters and growth of health science programs to provide economic impact, improved health outcomes and enhanced cultural enrichment.
About Strategy+
The post Integrated planning: why medical schools need a joined-up approach appeared first on Without Limits.
]]>The post Surplus office space to cutting-edge laboratory: three refit considerations appeared first on Without Limits.
]]>The UK’s Life Sciences sector is a national success story. It supports almost a quarter of million jobs and generates £70 billion in economic value, and it is growing – fast.
This growth is in part thanks to historic – and continued investment. In the Spring 2020 budget, the government announced a commitment to doubling the amount of funding to Life Sciences. The sector is also in the spotlight as numerous organisations, from global pharmaceutical companies, to the Department of Health, Public Health England, academia and science parks collaborate on a vaccine against coronavirus. These efforts have also been backed by government, which has pledged tens of millions of pounds to scale-up research, particularly among start-ups.
This combination of factors means that the demand for suitable research and development facilities is rising exponentially, as there was a shortfall of space even before the current pandemic. Whereas constructing newly built premises is slow and carbon intensive, refurbishing existing office space offers a faster and more efficient solution. It’s a golden opportunity for commercial developers and public sector bodies to re-evaluate their existing assets to meet that demand, one that has the potential to deliver higher rental returns.
In this article we examine Life Science sector needs and why it is good time to repurpose surplus sites. We also share three considerations that asset owners can make when examining real estate portfolios.

Understanding sector needs
So, what exactly is the Life Science sector looking for? For most the answer is location, location, location. As traditional science disciplines blend with tech and digital science, life science companies are increasingly seeking out premises in areas where Innovation Districts are either established or emerging.
According to laboratory fit-out specialists Galileo Labs, “The nature of life science research is shifting to a collaborative model where co-location and open and accessible facilities for smaller science companies is required. Combining the academics with clinical staff as well as research and development (R&D) partners creates a unique ecosystem, making property in the area extremely sought after.”
With continued investment in rail infrastructure, Cambridge and London connectivity is supporting the growth of these life science/healthcare ecosystems, alongside Oxford, with activity in the capital centred round the Knowledge Cluster at King’s Cross/Euston as well as Imperial College’s Innovation District at White City. Other key areas in the UK include Alderley Park near Manchester, Innovation Birmingham near Aston University, and Edinburgh’s BioQuarter. Across the water, Belfast and Dublin both have thriving Life Sciences clusters, particularly with the convergence of technology and life sciences .
The UK is still adjusting to new remote working practices in relation to coronavirus, but the sector is very limited in terms of what can be done outside the laboratory environment due to the need for sterile spaces and the increasing use of artificial intelligence to process vast data sets at speed. Demand is therefore growing for a range of accommodation from small labs for start-ups to larger combined laboratory and office space for more mature businesses.
Crucially, life science companies are also moving more towards enhanced office environments with smaller areas of wet/dry lab content, as traditional analysis methods are being replaced by smart, advanced technology. This is good news for those looking to repurpose existing facilities because less floor space needs the structural and services modifications to accommodate wet/dry lab areas.
However, no matter what the size or type of accommodation, co-location remains a key draw.
Repurposing existing space can meet demand
The UK has significant unmet property demand for small and large purpose-built science space in key locations. Public sector organisations looking to improve or relocate well-located parts of their estates while at the same time disposing of more obsolete sites are in a strong position, particularly if they consider working with commercial partners.
Repurposing an existing office block (or other space) with the right design parameters for laboratory use is advantageous in many ways. The representative rental values in London for laboratory space can range between £70 – £125 per sq ft compared to those for office space which are £57.50 per sq ft, according to Galileo Labs.
From a sustainability perspective, refurbishment can deliver a 56 per cent reduction in carbon emissions compared to a new build facility – giving lab space strong eco-credentials that may be attractive to prospective tenants. Aside from sustainability, there are significant gains in terms of speed to market. In addition, refurbished space can be flexible enough to accommodate multi-tenant start-ups right up to more established operators, who may wish to rent entire floors.
Here East, formerly the Media Centre for the 2012 Olympics, is a good example of an innovation and technology campus for start-up companies. Granta Park, a science park in Cambridge, has also undertaken studies into repurposing its existing space.
Three considerations
Here are three considerations when refitting space to a laboratory environment:
1/Consider slab heights and risers
An initial viability needs to quickly determine the slab-to-slab height of a building to establish whether there is enough height to bring in additional services, such as risers. Typically, a lab storey height would be 4.1 to 4.5m high (top of slab to soffit) allowing for the vertical distribution of air across the floor plate, compared to an office which is more likely to be 3.6m to 4.2m. Older properties such as telephone exchanges, banking halls and financial institutions generally lend themselves to this configuration, due to their dense frame and generous storey heights. Equally, warehouses, industrial premises and even shopping malls could be considered.
A solution to lower storey height buildings is to create greater density of internal risers and plant room space.
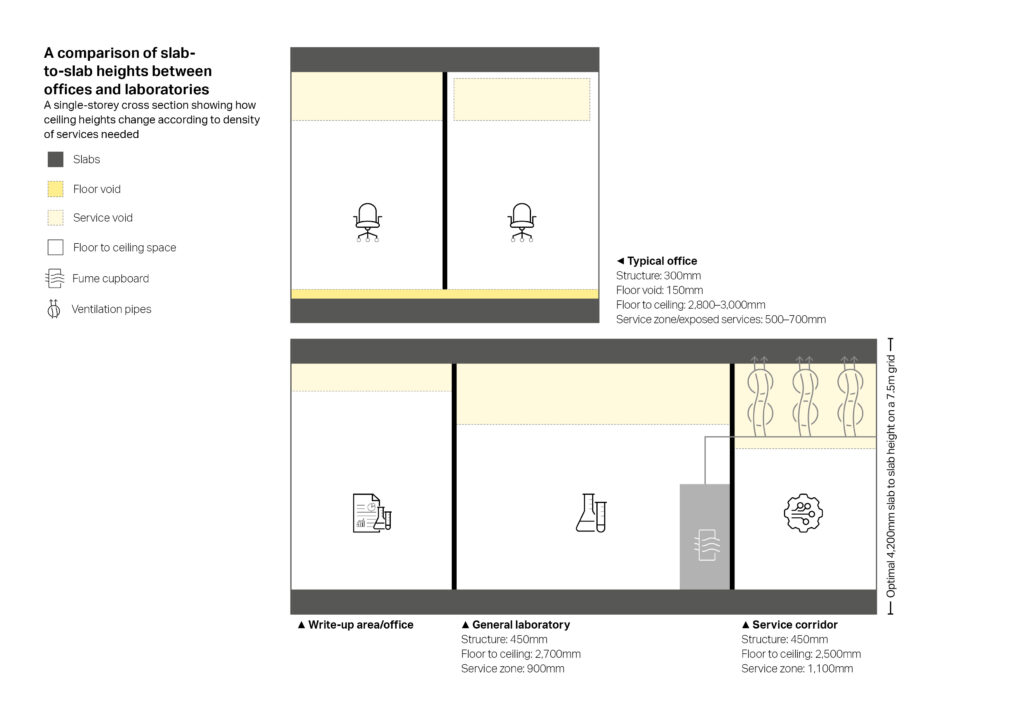
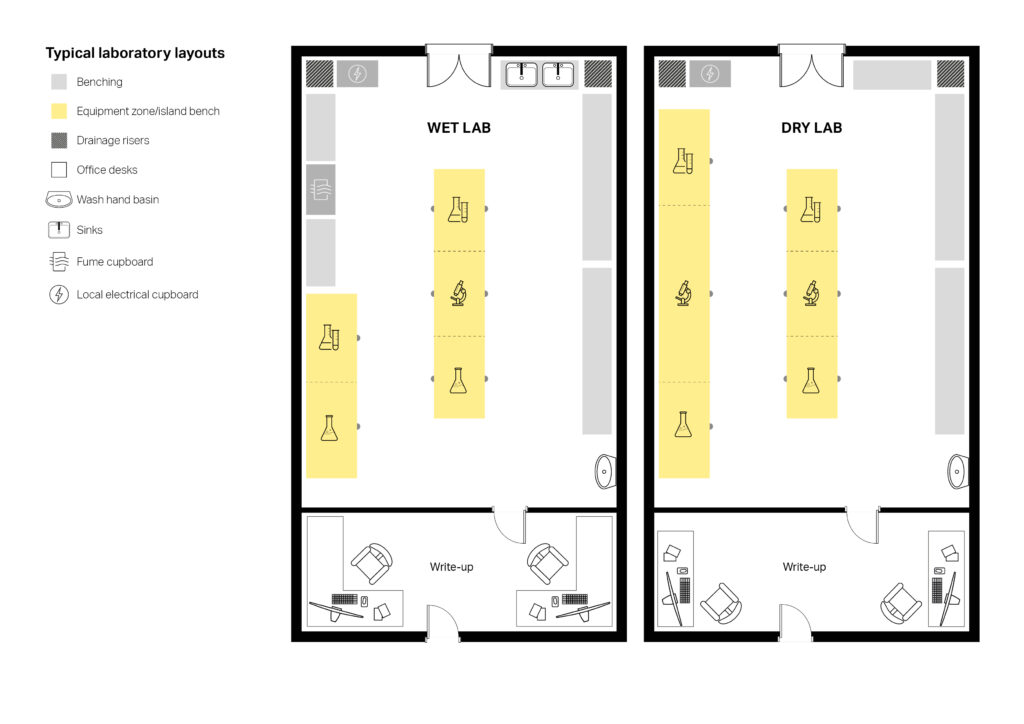
2/Take advantage of financial incentives
There are specific tax benefits associated with research and development (R&D). The capital cost of construction works to create dedicated research facilities for owner-occupiers benefits from 100 per cent capital allowances. Any innovative design or construction solutions to overcome site-specific scientific or technological uncertainties may qualify for R&D tax credits. These provide an enhanced (or super) deduction of 230 per cent for eligible staff costs for SMEs, or a 13 per cent ‘above the line credit’ for large companies.
3/Factor in wellbeing
Facilities with roof terraces and other recreational zones will be highly sought after, especially in urban areas. Scientists work in controlled environments so break out areas such as wellness/contemplation rooms and outside spaces will be in demand. These spaces can also be safely adaptable to serve a variety of functions in line with government distancing guidelines.
A golden opportunity
The case for refurbishment has never been stronger, and not just because it is a low carbon alternative to building new premises. It is also cost-effective and has the benefit of faster speed-to-market delivery, as well as being an opportunity to unlock assets in high-demand locations.
More space is clearly required to enable the life science sector to grow and refurbishing existing assets can help meet the demand for well-located, well-equipped laboratory space, while providing healthy returns.
The design and construction industry still has some way to go in communicating and demystifying the office-to-lab refurbishment process and increasing awareness amongst asset owners that they have a golden opportunity to maximise their underutilised or poorly performing assets. However, the case for office to laboratory refurbishment is strong and, as a result, we expect confidence amongst asset owners to grow.
With thanks to AECOM’s Josh John, Senior Project Surveyor and Lewis Peacock, Associate for their contributions to this article
The post Surplus office space to cutting-edge laboratory: three refit considerations appeared first on Without Limits.
]]>The post Healthcare planning and emergency response: the case for choosing modular solutions appeared first on Without Limits.
]]>Health services around the world have been operating under immense pressure due to the coronavirus pandemic, which has come on top of the usual seasonal surges that tend to stretch systems to the max. As the world waits for a vaccine, it has become clear that practical contingency plans and the creation of additional capacity to provide facilities in an emergency are crucial. In response to initial waves, additional emergency facilities were built at speed to cope and the use of modern methods of construction were key to their effective delivery – and can be in the future.
Modular Integrated Construction is a construction method that uses free-standing integrated modules ― complete with finishes, fixtures and fittings ― which are manufactured in a factory and then transported to site for installation in a building. The use of MiC in healthcare is not new: organisations first used prefabricated units for individual services such as outpatient and temporary wards or operating theatres to create additional capacity
Additionally, Design for Manufacture and Assembly (DfMA) is vital to appreciating the benefits of repeatable design to the healthcare sector. DfMA is already widely used in sectors such as the automotive and consumer-products industries, where large numbers of high-quality components are needed. In construction, DfMA can be used to manufacture components such as concrete floor-slab elements or partition walls to a standard specification in a factory, before they are brought onsite. Or, DfMA can be used to manufacture the parts used to assemble entire prefabricated units, such as temporary wards or bathroom pods and include Mechanical, Electrical and Plumbing (MEP) components in MiC.
Over the years, the industry has made huge strides, tailoring the facilities to the needs of clients, increasing standardisation of rooms, the material and manufacturing of the building engineering and equipment and improving the quality of the products. MiC facilities in healthcare can now be seen in the provision of isolation rooms and wards, critical care units, high-dependency units (HDU), community facilities such as family planning clinics, GP surgeries, mobile MRIs, hospital wards, clinical departments, doctor’s surgeries, surgical theatres and operating rooms, modular office spaces, reception areas, clean rooms and laboratories.
In this article, we discuss the wider benefits of adopting MiC and DfMA into general hospital planning and the construction of permanent hospital facilities, and how those benefits can be leveraged to enhance Emergency Preparedness Response and Resilience (EPRP) strategies, while sharing global examples.
How DfMA helped the UK respond to coronavirus
While DfMA and MiC have not yet been fully adopted into mainstream healthcare planning in many parts of the world, the UK has been using them for the last 30 years.
At the Royal Stoke University Hospital, a modular 12-bed critical care unit that included an isolation unit was delivered in just 24 weeks while normal working operations at the hospital continued. More recently, AECOM designed and provided building engineering services on a dedicated cancer centre in Liverpool. Thirty per cent of The Clatterbridge Cancer Centre’s structure comprised modular components, ensuring high build quality, reducing onsite timescales and reduced onsite health and safety risks.
These techniques were also used to deliver the NHS’s temporary emergency critical care hospitals, known as Nightingale Hospitals, that were commissioned during the initial pandemic response.
AECOM collaborated on the construction of the NHS Louisa Jordan hospital in Glasgow, which took just three weeks. In an interview for Building Magazine, Graeme Watson, project director at AECOM, explained how repeatable design sped up procurement, saying: “We assessed what we needed the most of and procured those products in the first couple of days. Having immediate access to clinicians meant they were able to see and touch the bedhead luminaires and make decisions there and then, so we could order 1,200 luminaires within minutes.” He added: “Traditionally, healthcare projects have initially been architecturally led, but incorporation of repeatable design, modular and off-site from the start brings quality, speed of delivery and safety benefits.”
Case study: Grange University Hospital, Gwent, South Wales
The early completion of the £350 million 560-bed Grange University Hospital in Gwent, South Wales, was made possible thanks to the use of modular construction and off-site methods. Off-site and DfMA methods were already being used, but when coronavirus hit, the construction team were asked if they could fast-track the build programme. Just four weeks later, the hospital took possession of 50 per cent of the space which enabled the hospital to provide support during the crisis, which otherwise would not have been possible had a standard build approach been planned.
The DfMA healthcare component and the associated workforce labour savings of 237,099 working hours (the equivalent of 5,927 working weeks) provided a 23 per cent overall planned programme saving. 821 precast columns where installed, which led to an 85 per cent savings in working hours and 1200 precast wall modules were installed, leading to a 95 per cent savings in working hours.
The formal completion of the hospital is expected in November 2020. Once fully open, it will provide complex critical care treatment for more than 600,000 people in Southeast Wales.

The many benefits of a modular approach
Given the long-term success in the UK, there is a strong case for integrating repeatable design methods into healthcare planning elsewhere around the world both during this current coronavirus pandemic, as well as in the future.
There are many benefits. Modular facilities can help with managing demand and capacity, surge, and winter pressures and in times of emergency. Projects are typically completed 50 per cent faster, with less accidents on-site and quality is ensured by the fact that production takes place in a controlled factory environment. There is less impact on the ‘live’ operations of a hospital or healthcare facility as these facilities can be delivered much faster than traditional on-site construction.
What’s more, the shorter time frame also results in less impact on existing healthcare facilities, reduced vehicle movements and waste on-site, savings on energy costs and an overall more efficient use of public funds.
The MiC volumetric units or DfMA component parts can be brought to site during off-peak times, with much of the construction happening in the factory. This reduces on-site construction waste, lowers safety incident levels and makes it less intrusive to staff and patients nearby.
Procurement is often done via government frameworks ― often resulting in a five percent reduction of standard cost rates as well as faster appointments and delivery of healthcare facilities made as a result of direct awards or mini competitions.
Furthermore, with MiC, there are already various repeatable room designs and clinical layouts available – a real benefit for those working in or managing healthcare facilities. This can be particularly useful in an emergency when there is no time for design and ready-made solutions are most practical. When time permits, however, suppliers can tailor the clinical spaces to individual needs. MiC can be used across all healthcare sectors including acute, primary care and mental health.
What’s more, the life expectancy of these buildings is approximately 70 years and can be adapted to meet future clinical need or re-used for another service ― particularly useful in transforming them for clinical or administrative services.
A worthwhile investment
As coronavirus continues its hold on countries around the world, solutions are still being explored to create sufficient isolation, quarantine and critical care facilities, regardless of whether they are temporary, permanent or a refurbishment of existing areas. MiC and C solutions bring cost and time savings, factory-level quality, as well as lessened impact on live healthcare sites and safety to allow clinicians and managers to focus on continued provision of patient care.
These methods provide an alternative way to quickly and safely build additional capacity to meet the urgent and growing demand for facilities faced by healthcare systems today – both in emergencies and as part of a long-term programme.
Case study: Outpatient clinic, Hawaii, United States
In western Oahu, Hawaii, modular prefabricated construction methods were used to complete an outpatient clinic including most of the interior partitions and the primary structural frame. The partitions used in the provider offices and patient exam rooms contain prefabricated modular electrical systems, prefinished cladding, plumbing systems, glazed doors and storefront windows as well as accent art graphics. This wall system is part of a programme to standardise elements across all provider facilities.
At the same time, the client is also creating a complete computer 3D model including heating, air conditioning and ventilation (HVAC), electrical, plumbing and finished wall systems. Ultimately, they will provide these models to each of their project teams so that architects can “plug and play” into their specific conditions and know that they are documenting a complete building that meets all of the client’s programmatic requirements. This increases efficiency in the design process and coordination of systems, while reducing capital costs for the benefit of the client’s overall insurer system.
The post Healthcare planning and emergency response: the case for choosing modular solutions appeared first on Without Limits.
]]>The post Transforming health and social care through digital technology appeared first on Without Limits.
]]>In April 2017, the Scottish BIM policy note set out how this collaborative tool that digitally captures all information related to a building should be adopted in public sector procurement. Since then, the implementation of BIM has become a key priority for HFS and NHSS. HFS has led on the introduction of BIM across NHSS through several pieces of work and the introduction of an NHSS BIM Development Group, now known as the Digital Estate Group. The group, in conjunction with HFS and consultancy support led by AECOM, have developed a BIM strategy.
This supports documents, templates and includes a training programme for NHS Boards to ensure the creation of a digitised information management process for those working on NHSS programmes. This enables consistency and facilitates collaborative working, which will in turn reduce waste and non-conformances. HFS and NHSS are prioritising the implementation of BIM across Scotland’s Health Boards.
With BIM fully embedded, NHSS is now creating a digital estates strategy. One of the key components of this is the digital twin — a shift from a deterministic to a more probabilistic, dynamic model.
Digital twinning
Via digital twinning, NHSS aims to link its physical assets (buildings and potentially end-users) to a digital representation, using data from sensors and analysing variables such as condition, efficiency and real-time status. This connectivity coupled with data analytics will reform facilities’ levels of operational effectiveness, generate extra insights from the digital twin to help reshape and improve services, support person-centred care, and improve outcomes in line with the ‘Digital Health and Care Strategy’.
The BIM process benefits individual NHS Boards by improving information management at a project level. It also has a significant impact at an organisational level overall. This longer-term vision supports the concept of a digital estate alongside the physical — a portfolio-wide collection of structured, indexed and searchable digital asset information, making it easy for a board to search, retrieve and make sense of its existing information. Over time this will help NHSS with future investment and better decision-making.
Seeing the bigger picture
Alongside recognising BIM as a tool to help deliver better hospitals and built assets, it’s important for users to understand how it can help improve service quality and efficiency, and the patient experience. For example, our strategic approach couples concepts, bringing processes such as BIM and Soft Landings together with technology to align building users’ objectives and operational functions, and support NHSS’s compliance agenda. Using BIM, digital simulations and analytics, we can then test the theoretical against the brief.
Four critical cornerstones
As part of our work advising HFS on its national approach and training material for Scotland’s Health Boards, we identified four cornerstone actions to help fully reap the rewards of a BIM approach:
1/Embed the UK BIM framework
It is important that all participants work from the same consistent set of standards and processes. To enable that, we recommend embedding and using the UK BIM framework, which comprises core standards backed with common processes and a suite of
enabling tools that, in combination, bring BIM deliverables to life. These focus on:
- Defined information requirements
- Collaborative working practice
- Data exchange and validation
- Security-minded digital working
- Better outcomes and end-user value (digital reality checking and a Soft Landings framework approach).
2/Ensure collaborative working – use of Common Data Environments (CDE) and workflows
The NHSS estate contains a colossal amount of information, which can be challenging. To tackle this, it’s essential to establish an Information Management and Common Data Environment (CDE) strategy that follows an agreed information hierarchy, covering how directories and folders should be structured along with agreed workflows and naming conventions.
3/Take a security-minded approach
As the use of digital data increases, so do the security risks associated with physical controls, staff behaviour, unauthorised access, and manipulation and sharing of data, information and systems. In a healthcare setting, you must consider the security of staff and patients, built assets, and the services delivered from those built assets, as well as the data and information that staff hold or can access. As a priority, you need to develop, implement and enforce a strict policy covering access to, and permissions for, sensitive information and project data.
The UK BIM Framework document, PAS 1192:5 ‘Specification for security-minded building information modelling, digital built environments and smart asset management’ details appropriate and proportionate measures you should take to manage security risks for a built asset, in whole or in part, asset data and information.
4/Use Soft Landings to maintain value throughout the lifecycle
Soft Landings (SL) is an essential element of the design and construction process. It maintains the golden thread of a building’s purpose through to delivery and operation, via early engagement with end users, the inclusion of a SL champion on the project team and, importantly, a clear commitment to aftercare post-construction. The SL approach aims to improve building performance by “aligning the interests of those who design and construct an asset with those who subsequently use it”.
It works to smooth the transition from design and construction into the operation and use of an asset, to make sure that operational performance is optimised. To enable that, these transitions must be considered from the earliest stages of a project right through to completion, rather than just at the handover stage. We combine BIM and SL to enable aspects such as reality checking and capturing digital information throughout the entire lifecycle. This information can then be used, for example, to test maintainability and support better stakeholder engagement through data-rich virtual environments.
What BIM success delivers
Successful and consistent BIM implementation across all Boards will facilitate and strengthen knowledge sharing across NHSS, support better decision-making and deliver greater efficiencies through the design, construction and operational stages of a project. Equally important, it will help the Scottish Government deliver the objectives of its ‘Digital Health and Care Strategy’, improving patient care.
CASE STUDY
AECOM’s BIM and Information Management specialists have been advising Scottish Futures Trust, the Scottish Government’s infrastructure centre of expertise, and HFS for several years and were involved in originating the NHSS BIM Strategy. Alongside this, our Global BIM Consultancy Director, David Philp — who in a previous role has been involved in the development of HFS’s initial BIM Level 2 strategy — was seconded to support the Government policy implementation as chair of the Scottish BIM Delivery Group.
Crucially, our team contributed to the development of an innovative BIM portal that supports public sector procurers who adopt BIM on new construction projects.
Currently, we are advising HFS on the introduction of BIM across NHSS and NHSS Digital Estate Group.
The post Transforming health and social care through digital technology appeared first on Without Limits.
]]>The post Costing primary care facilities appeared first on Without Limits.
]]>The NHS is under immense strain, battling staff shortages, historic underfunding, and a growing UK population with complex health needs. Until recently, the majority of spending has been applied to areas in acute need as well as day-to-day running costs. But attention is now turning to improving primary care buildings that house vital front-door services such as GPs, community pharmacies, dental and health services.
The NHS Long-Term Plan, a 10-year blueprint, sets out commitments that will fundamentally change how these services are delivered. The goal is the creation of “fully integrated, community-based healthcare”. It’s a concept designed to make physical assets work harder and more effectively, while encouraging a more holistic, preventative approach to the nation’s health.
As a result, primary care funding is on the rise. The planned distribution of NHS funding for 2019/20 will see almost £80 billion allocated to Clinical Commissioning Groups (CCGs) across England for local health services. This represents a chance for primary healthcare buildings to receive the investment they need to meet localised healthcare demands.
The digital opportunity
The NHS has called for a complete overhaul in how primary care is accessed, with a digital-first approach. However, successfully integrating digital services into physical infrastructure is one of the biggest tasks facing developers of new primary care projects. To make digital consultations become the new normal, primary care physical assets now need to enable this.
Shortening the patient journey through the physical health space via digital technology can have major health implications by saving time and enabling more accurate diagnosis, thus improving health outcomes and patient satisfaction. Furthermore, effectively incorporating digital services into physical assets can also mitigate two of the biggest issues facing the NHS: staffing and funding.
Flexibility is imperative
There is now a shift towards bigger, more flexible and interactive buildings that can be repurposed quickly. For example, a primary care building could be used as a community meeting space in the evening but if there’s a sudden, pressing need and demand for evening appointments increases, then the space could be freed up for treatment instead. As the coronavirus has made clear, there is a public health imperative to be able to reduce or expand the number of people visiting physical primary care facilities.
However, providing such high levels of adaptability brings challenges. Flexible spaces still need to be able to offer appropriate levels of containment and privacy quickly so healthcare providers can engage with their patients one-on-one or in confidence if required.
Sustainability
Sustainability is a key driver of change in the design and costing of the NHS’s primary care assets. As environmental scrutiny is heightened and zero carbon goals emerge, standards have rapidly shifted from design nice-to-haves into essentials. New-builds have different sustainability criteria to refurbishments: newly built facilities need to achieve a BREEAM Excellent rating whilst a refurbished scheme has to achieve Very Good.
Furthermore, new models are emerging to improve the sustainability of all asset types. Community Health Partnerships (CHP) has spent more than three years working with a team of advisers, including AECOM, researching the potential benefits of ultra-sustainable design not only to improve the user experience but also to reduce whole-life cost of ownership.
NHS England is thought to be the only healthcare system in the world that is routinely reporting on its greenhouse gas emissions. This year it is due to release a report examining the scale of its carbon footprint, which will also provide a timeline and plan towards the organisation achieving net-zero carbon emissions. It follows that CCGs will be increasingly expected to account for and reduce their energy usage and carbon output.
Cost breakdown for an example fit-out
Our cost model is for a Category A fit-out of a shell and core development into a primary care health centre in England, for GPs, community nurses, midwifery services, mental health services, social services and support services. View and download the cost model here.
An edited version of this article first appeared in Building magazine in June 2020.
The post Costing primary care facilities appeared first on Without Limits.
]]>The post Rapid repurposing: facility strategies for airborne disease outbreaks including coronavirus appeared first on Without Limits.
]]>Given the scale of the coronavirus pandemic, projecting need for and accommodating beds is difficult beyond one to two weeks. With this in mind, our recommended first response is to free up additional capacity within that one- to two-week timeframe using existing resources that can be rapidly modified for quarantine, treatment, and recovery. This can be done with minor modifications to existing hospitals, followed by assembling equipment solutions from non-traditional supply chains (residential or commercial rather than specialist healthcare supply chains) for ad hoc quarantine units in high school gymnasiums or other large assembly facilities.
Rapid repurposing
There are strategies that you can deploy now, using facilities that exist and equipment that is available in your community to fight Coronavirus immediately. We can help.
Preparing a response
Hospitals are not set up to deal with the anticipated surge in patients, meaning ad hoc solutions will be required both to address this outbreak and to allow hospitals to continue treating patients suffering from other ailments..
With coronavirus and other airborne virus outbreaks, there are two types of patient: presumptive cases and known cases. Both groups have different facility requirements and put unique stresses on the hospitals.
There are two critical levels of containment to consider:
- Quarantine: Containing presumptive-case patients from each other and the general population; and
- Isolation: Containing confirmed-case patients from the general population.
Confirmed-case patients can be housed together en masse while presumptive-case patients must be individually quarantined.
For healthcare systems and for our communities in general, finding more available and readily adaptable space becomes a priority – often in non-traditional places. Readily adaptable space can include facilities outside of the traditional healthcare portfolio. The following could become available and be adapted using our quick implementation solutions:
- School closures mean high school or college gymnasiums can offer durable, cleanable surfaces, large open spaces and locker rooms.
- High school or college campuses often have ample open outdoor space to accommodate temporary structures, emergency power and parking
- Hotels and universities/colleges dormitories can be converted using recommended strategies for patient and treatment accommodation.
- Community centers can offer accessible facilities, with durable, clean surfaces, with separate room for those with cognitive vulnerabilities.
To contain this outbreak, and defend against future outbreaks, we must respond in three stages:
- Near-term (7-14 days): to ensure immediate response at the treatment facility level requires nominal readiness based on projections of patient load;
- Mid-term (14-28 days): to ensure large-scale readiness requires short-term response at a larger community level based on projections of patient load;
- Long-term: to ensure appropriate-scale readiness for future outbreaks requires response at the population at large level.
Immediate containment response measures
Adapting existing spaces: immediate response at the treatment facility level to ensure nominal readiness based on near-term projections of patient load.
Hospitals can convert blocks or wings of existing non-critical patient rooms to quarantine or isolation rooms by changing the ventilation and the room entry conditions and standard operating procedures (SOPs). A negative-pressure room is required to isolate a patient who is either suspected of having or who has been diagnosed with an airborne infectious disease so that the number of airborne infectious particles is reduced to prevent cross-infection of other people.
Isolation rooms need to be negatively pressurized to their adjacent, communicating spaces, and they need to have a buffer zone between the isolation room and the corridor outside of the space. Where true anterooms aren’t present to serve as this buffer zone, polyethylene plastic sheeting (Visqueen®) can be hung from the ceiling to create a space where personnel can spray down their personal protective equipment (PPE) with disinfectants such as Lysol® or Virkon®. This allows time for air changes in the anteroom, before removing PPE at the point of exit. While traditional anterooms are positively pressurized to both the corridor and the patient room, this is not required if adequate use of SOPs and disinfectants are employed.
Adapting what exists
- Readily convert blocks or wings of non-critical patient rooms by changing ventilation, entry conditions and SOPs.
- Train, retrain and use occupational safety point-and-call methods real time to eliminate errors.
- Create a network of support facilities through appropriate community buildings retrofitted for treatment.
The main patient room can be re-balanced as negatively pressurized if the heating, ventilation and air conditioning (HVAC) system is non-recirculating. Otherwise, windows should be opened or removed, and temporary fans shall be installed at the window, and sealed up with a barrier such as rigid plastic or epoxy-painted plywood.
The window barrier should be sealed around the edges and at the point of ventilation penetration to ensure a tight containment boundary. The use of tell-tales at door undercuts is advised for a quick visual check of directional airflow.
This room setup will work for presumptive- and confirmed-case patients. Room signage, SOPs, and other guidance should be marked on each patient room door as clearly as possible to minimize human error. Training, retraining, and using the pointing-and-calling method for actions as they occur is recommended to eliminate errors as well.
Getting technical
A minimum MERV-16A filter should be applied to the exhaust airstream and shall be operated at a velocity of less than 500 fpm. For the room balance, the ideal differential pressure is between -0.05” and -0.10” w.g. from the corridor to the patient room.
Short-term containment response measures
Short-term response at the community level to ensure large-scale readiness based on mid-term projections of patient load.
As hospitals begin to reach capacity, municipalities should work with healthcare organizations to make a network of support zones that are typically distributed with existing community densities. To further expand your community’s capacity to quarantine presumptive cases, explore opportunities to transition other building types that are similar in structure to a hospital patient wing, including university dormitories or hotels, where similar strategies could be quickly deployed. Additionally, academic health centers pose an opportunity to have nearby healthcare and flex space using large open spaces like gymnasiums and dining halls.
Each location should be setup with check-in, open-space queueing, and triage. From here, presumptive-case patients should be taken into a dedicated isolation bay. Several bays can be co-located in a large area such as a cafeteria or dining hall. Isolation bays can be constructed with PVC plastic frames and polyethylene plastic sheeting (Visqueen®). Confirmed-case patients should be taken into a large isolation suite, such as a gymnasium. Here, the entire space can be open to the patients who are co-located en masse.
Getting technical
Each isolation bay must be negatively pressurized with MERV-16A filtered exhaust that is operated at less than 500 fpm and is not recirculated into any space. Each isolation bay is provided with an ante room for donning and doffing of PPE. The negative pressure of the isolation bay will cause air to cascade from the large open space, through the ante room, and into the isolation bay. A minimum of 500 CFM is recommended for each isolation bay. In large isolation suites, the entire space is conditioned and ventilated without recirculation to maintain a pressurization between -0.05” and -0.10” w.g. from the clean spaces to the isolation suite.
PVC and polyethylene plastic sheeting can be used to create clean corridors between entry and exit points and the locker spaces that are to be used by the healthcare workers. The locker rooms are where the workers can change from street clothes into PPE, and then back into street clothes at the end of the day. No scrubs or PPE should be taken off-site. Healthcare workers should shower before changing into street clothes and leaving the site.
Provide supporting site infrastructure: Emergency power can be provided for critical equipment such as ventilators via a generator or a dedicated uninterruptable power supply (UPS) at each point of use. Waste and materiel flows should be mapped to avoid cross-contamination. Further, care should be taken to use waste bagging and wipe-down sterilization until the waste can be autoclaved or otherwise safely sterilized.
Justice facilities
As with the community at large, the criminal justice system will need to find more available and readily adaptable space for treatment options as a priority – often in non-traditional places.
With minor modifications existing justice facilities could be repurposed to provide ad hoc quarantine units in alternate spaces such as day rooms, food service facilities and/or gymnasiums. These can be furnished, according to need, with equipment from non-traditional supply chains (residential or commercial rather than specialist healthcare supply chains), scaling up as required.
The following spaces could be adapted using our quick implementation solutions:
- Gymnasiums, day rooms, classrooms, or food service areas within secure facilities can offer durable, cleanable surfaces and large open spaces; and
- Dormitories and cells can be converted using recommended strategies for patient and treatment accommodation.
The main in-custody patient room can be re-balanced as negatively pressurized if the heating, ventilation and air conditioning (HVAC) system is non-recirculating. Otherwise, windows can be removed, the openings secured, and temporary fans installed. The use of tell-tales at door undercuts is advised for a quick visual check of directional airflow.
This room setup will work for presumptive- and confirmed-case patients. Room signage, SOPs, and other guidance should be marked on each patient area door as clearly as possible to minimize human error. Training, retraining, and using the occupational safety pointing-and-calling method for actions as they occur is also recommended to eliminate errors.
As treatment facilities begin to reach capacity, jurisdictions might consider working with the facility administration and healthcare organizations to create a network of support zones encompassing the detention facility and the wider community. Academic health centers could also be part of this network, with the advantage of having auxiliary healthcare professionals available.
AECOM can help
Each facility is different, so please consider allowing AECOM to answer any questions you might have, and to assist as your partner in immediately addressing your most pressing needs. Our staff of engineering consultants is ready to help and guide you through the process, modifications, SOPs, and start-up.
Distributed across the United States, AECOM’s teams are ready to support your community healthcare needs with the following services:
- Disaster preparedness, response, and recovery planning and strategy development
- Disaster response program management
- Access to specialist expertise to support your in-house teams.
- Communication and outreach
- Solution design, development and delivery
- Operational facility re-programming
- Transportation management to ensure containment during transfer
- Business continuity consulting
- Microgrid design and delivery
- Post-event cleanup and transition consulting
Please contact us to discuss how we can help.
The post Rapid repurposing: facility strategies for airborne disease outbreaks including coronavirus appeared first on Without Limits.
]]>The post Dark Waters: film about PFAS pollution stirring debate in Europe appeared first on Without Limits.
]]>Until recently PFAS haven’t had much attention in Europe – at least not in comparison to the fierce debate in the U.S. and Australia. In production since the 1940s, per and polyfluoroalkyl substances, commonly known as PFAS, are found in everything from pizza boxes to firefighting foam. Some PFAS don’t break down, and can accumulate over time in humans, animals and the environment. In some cases, they’ve been known to leach into drinking water and appear in wastewater.
Whilst toxicity levels are uncertain, PFAS chemicals have been linked to weakened childhood immunity, thyroid disease, cancer and other health problems. Industries such as oil and gas refineries, chemical and industrial companies, landfills, ports and harbors, defense, aviation, and water treatment companies all face PFAS issues that require identification and intervention.
In the U.S. and Australia, high profile cases and class actions have raised public awareness and regulatory attention. In Europe, regulation and enforcement is evolving, with stricter rules anticipated.
What countries are taking action?
Across Europe awareness and approaches differ widely. Here are some examples:
Scandinavia – Norway, Sweden and Denmark are paving the way, and have regulatory standards defined for several PFAS compounds in soil and/or groundwater. Some of their drinking water standards for PFAS-related compounds PFOS and PFOA are the most stringent in Europe.
The Netherlands– Public awareness about the risks from PFAS has been sparked by several high-profile cases. Additionally, the Netherlands has always been comparatively more proactive compared with other European countries with regard to the regulation of contaminated land.
Italy – PFAS are gathering attention, in part driven by a case in the Veneto region in northern Italy where it has been estimated that up to a couple of hundred thousand people in a catchment may have been exposed to PFAS in their drinking water. The original concern related to a now defunct PFAS chemical production facility in northern Italy. Monitoring and health surveillance programmes have been put in place and further research continues, in part funded by the EU Life programme.
UK/Great Britain – In 2005, a fire broke out at the Buncefield oil depot. To bring it under control, firefighters poured vast quantities of the chemical onto the fire, contaminating the water table. The incident triggered increased concern on the potential for PFOS to impact drinking water supplies. The Drinking Water Inspectorate (DWI) introduced tiered drinking water standards for PFOS and PFOA in 2009. In the Channel Islands, dependencies of the British Crown, PFAS is firmly on the radar with well-known cases at both Guernsey and Jersey airports.
Is there a solution for PFAS?
A major concern about PFAS is that the very stable nature of the perfluorinated compounds means they are difficult to destroy. Although absorption or separation methods can be used to protect drinking water supplies, traditional remediation techniques cannot break the carbon-fluorine bonds in PFAS except through high-temperature incineration. This last method can be costly due to the need for transportation to a suitable facility. Several operators are therefore seeking better and more cost-efficient ways to deal with PFAS.
For more than a decade, AECOM has been looking at ways to treat PFAS in a cost-efficient manner on-site. Having worked on more than 300 PFAS projects globally, and successfully managed two of Australia’s precedent-setting PFAS investigations, the destructive treatment technology (DE-FLUOROTM) we’re developing is at the forefront of efforts to destroy these potentially toxic chemicals.
What’s ahead for Europe?
Because of their historic widespread use, PFAS touch many parts of our business and social communities. Regulations protecting human health and the environment from the potentially negative effects of PFAS are becoming increasingly stringent. This could continue as additional scientific information regarding the many thousands of PFAS is collected.
AECOM is helping inform industries and regions about PFAS, and the remediation and management solutions available.
The post Dark Waters: film about PFAS pollution stirring debate in Europe appeared first on Without Limits.
]]>The post Rethinking how we tackle air quality and health appeared first on Without Limits.
]]>Local air quality is getting at lot of air time as awareness about the impacts of pollutants on our health, lives and planet increases. However, the tools and guidance we use to manage local air quality and tackle air quality issues derive from decades-old studies and incremental updates to legislation.
The result is rigid appraisal methods focused on legal compliance with sometimes semi-arbitrary thresholds and limits based on simplistic ideas of where people spend time.
As air quality professionals we should be challenging this irrational and discriminatory situation. We need to consider what level of pollution people are exposed to, irrespective of what activity they are involved in or whether they are at home, at work or at leisure in a public place. We also need to consider how to take better account of those who are more sensitive to the health effects of pollution.
Health and Legislation
Europe lacks a holistic view of the effect of air pollutants on the population due to a disconnect between ambient air quality legislation, public health responses, and workplace exposure to air pollutants. Exposure to air pollutants experienced at work, at home or in public places are treated differently. We also do little to consider air quality in conjunction with factors such as health, poverty, social mobility and education; and we do little to understand the implication of time spent in different locations.
For example, due to a disparity between environmental and occupational regulation the customer buying a coffee in a railway station concourse is subject to a far lower pollution threshold than the barista serving the coffee. So, we allow the barista to inhale a far higher dose of pollution during the course of a day than the customer.
Take another example: we are very careful when it comes to allowing new houses to be built alongside a polluted road, yet offices and shops can be built along the same road with no concern for the effect of the pollution on the office worker or shop assistant.
Health and Behaviour
Understanding of air pollution and our exposure to it is improving. For instance, we know that indoor air pollution can be exacerbated by energy-efficient building regulations that limit air changes, or by reliance on mechanical ventilation from polluted external locations that have been determined by construction and design needs rather than health or environmental concerns. We also understand the benefit of issuing alerts and advising people to alter their behaviour – this is particularly useful for asthma sufferers.
Our daily lives are so varied, but our understanding is limited about the difference in exposure between those who walk, cycle, drive or take the bus or train to work, for example. We don’t know how opening a window or altering car or bus ventilation affects our exposure to pollution. We do attempt to address air pollution in specific situations such as railway stations, but even this doesn’t look at the different ways people within the space could be affected.
The result is that we focus our efforts on rigidly defined locations based on static data sets such as address point data. We don’t look at the individuals who use that space and how they actually spend their time.
We need to understand how, where and when critical population groups move and behave in order to truly attribute health-response effects that recognise not only the level of exposure but also the sensitivity of individuals to air pollution.
Big Data Solutions
Big Data technology gives us the ability to analyse information from data sets that are too large or complex to work with using traditional techniques. For the purposes of this article, one key advantage of this technology is that it allows us to anonymously track individuals as part of larger populations. It is routinely used to inform transport policy, using journey origin, destination and travel mode, and can make links to qualities such as health, wealth, education.
In reality, these are not rigid and discrete indices but truly holistic values. Increased wealth tends towards higher car ownership, greater range of travel, and higher levels of education and social engagement, resulting in better overall health and lower sensitivity to pollution[1].
It must be recognised that those most sensitive to changes in air quality are also least able to respond to the measures required to improve it. For example, a societal shift to low-emission vehicles would benefit poorest individuals most – but they would be least likely to afford it[2]. Sensitivity is therefore needed when designing interventions, with care taken to understand how they will affect behaviour and lifestyle, and not just focus on air quality in isolation.
Ultimately, a holistic approach that includes social and behavioural feedback would inevitably change how we appraise potential interventions. A holistic approach would use air quality improvement as a mechanism to promote change and blur the lines between specialist disciplines to deliver an informed consideration of the knock-on effects.
[1] https://airqualitynews.com/2019/08/08/viewpoint-air-pollution-and-fuel-poverty-shouldnt-be-tackled-in-isolation/
[2] Joanna H. Barnes⁎, Tim J. Chatterton, James W.S. Longhurst (2019) Emissions vs exposure: Increasing injustice from road traffic related air pollution in the United Kingdom, Air Quality Management Resource Centre, University of the West of England, UK, Transportation Research Part D 73 (2019) 56–66
The post Rethinking how we tackle air quality and health appeared first on Without Limits.
]]>The post Evidence-based design in practice appeared first on Without Limits.
]]>Improving patient wellbeing and recovery times, reducing staff stress and infection control remain key priorities for today’s healthcare providers. While these can be influenced by a number of factors, such as quality of care and available resources, the correlation between good healthcare building design and improved medical outcomes is becoming increasingly recognised.
Informing and improving design
Healthcare design has changed enormously over the past 20 years. One of the biggest changes we continue to see is the application of evidence-based design (EBD). The Center for Health Design (CHD) defines EBD as, “The deliberate attempt to base building decisions on the best available research evidence, with the goal of improving outcomes and of continuing to monitor the success or failure for subsequent decision-making.” This is where human behaviour studies and evidence of the psychological effects of healthcare environments on patients and staff are used to inform and continuously improve healthcare facility design.
Creating healing environments
The movement towards EBD is improving the quality of hospital environments, making spaces more pleasant and comfortable, and using positive distractions, such as views of nature and uplifting artwork. Reducing environmental stressors, such as noise, and improving wayfinding is helping to create healing environments’, resulting in faster recoveries and improved patient outcomes.
Reducing staff stress
EBD also improves the staff experience by making workflows more efficient and providing a lower-stress environment. For example, evidence shows that providing healthcare staff with window in workrooms significantly reduces the number of medical errors. And Rollins, J.A. (2004) confirmed that daylight positively impacts patients and staff. In addition, having a view is associated with shorter patient stays, higher satisfaction with nursing care and a decrease in the use of medications. While environments, such as emergency departments, can be high-stress and a coffee break with a view can help staff clear their head and return to work more focused on their patient’s wellbeing.
The case for EBD
A growing number of studies and reports support these positive claims and the overall case for EBD. Perhaps most recognised is a View through a window may influence recovery from surgery, by Roger Ulrich, the world’s most cited and influential evidence-based healthcare design researcher. His research found that patients placed in recovery rooms with a window facing a natural setting had shorter hospital stays. According to Ulrich, “Views of vegetation, and especially water, appear to sustain interest and attention more effectively than urban views.”
In another paper by Ulrich, Effects of Healthcare Environmental Design on Medical Outcomes, he discusses the traditional design of healthcare facilities to be functional and efficient without considering the psychological needs of patients, visitors and staff. He touches on the correlation between poor design and the wellbeing of patients, concluding that the designs of healthcare facilities need to consider more than just function, “[A] critically important goal of designers should be to promote wellness by creating physical surroundings that are psychologically supportive.”
EBD in practice: King Hussein Hospital, Amman, Jordan
The new AECOM-designed King Hussein Hospital, part of the first phase of the King Hussein Medical City (KHMC) expansion, is the largest medical centre for the Royal Jordanian Armed Forces. It has 940 beds, including 144 intensive care beds and a new 16-bed burn unit, 43 operating theatres and the country’s main Level-1 trauma centre with 125 treatment/exam rooms. While primarily serving armed forces personnel and their families, the new, 30-storey facility, which replaces the existing King Hussein Hospital, will become one of the main public hospitals for the city of Amman.
As lead designer, our challenge was to create an organised, efficient, easy to maintain and easy to navigate, visitor-friendly hospital. We used extensive research, including working with doctors and nurses to inform the following EBD decisions that would achieve each of these requirements, while also creating a “healing environment for patients, staff and visitors, supporting and driving overall improved medical outcomes”.
Enhanced wayfinding
Good wayfinding is a key element of reducing stress and a factor that must be considered from the early concept design stage. It was imperative that we organised the building’s form and services so that it would be visually obvious and intuitive to everyone who interacts with it.
Long, covered areas for arrival and drop-off accommodate many cars for both scheduled and emergency patients, while large expanses of glass call out the main entry lobby and other public spaces, providing good visibility for visitors as they approach the hospital. Inside, straightened-out corridors make the layout less maze-like and have views to the outside to help people orient. Also, referencing internal landmarks, such as nurse stations, reception desks and other architectural features, helps people remember their route.
Multiple visual cues for visitors, such as themes, materials and colour, define departments and zones. Patients also avoid having to go through one department to access another, reducing traffic and noise and increasing patient privacy. Meanwhile, integrated technology, such as digital signage and electronic management of patient movement through the facility, support wayfinding and patient flow.
Family-centred design
Families are often overlooked in healthcare design. But they are an active part of a patient’s care and play an important role in the healing process.
Today, patients and their visitors seek divisions of space that offer smaller groupings of seating for better privacy and comfort and, using the hospitality industry as a design reference, people like choice. As such, it was important to create a variety of smaller areas, allowing for a range of options that appeal to different ages, personalities and physical needs. Separating public areas from the hustle and bustle of ‘back of house’ activities will also allow for a more pleasant visitor experience.
Waiting areas include quiet lounge areas, and public areas provide plenty of seating both indoors and on outdoor rooftop terraces, with a coffee shop and public cafeteria on different levels. All of these take advantage of the hospital’s hilltop location to offer what should be some remarkable views of the city of Amman. There are also a couple of public spaces with café seating, where visitors can have a drink and surf the internet on their laptop, as well as children’s areas, which have playful child-scale furniture and are acoustically separated from adult spaces but within easy sight of parents.
Greater privacy and calming views
As mentioned previously, views of nature have been statistically proven to improve patient outcomes, so in the new King Hussein Hospital, the idea of patient rooms with views was central. All rooms are single bed, with a view out over the city, or a rooftop terrace. These also allow for better privacy, are more restful for patients and better for infection control. In all rooms, there is an area near the windows for family, with seating out of the way of the nurses and doctors. All patient rooms, and their en-suite toilets are accessible, as per the American ADA Guidelines; except for one 24-bed ward, which is specially designed to accommodate very large “Bariatric” patients, who have their own unique requirements.
Integrated technology
Technology has been used to improve convenience. Patient tracking screens let patients know when they can expect to be seen. Families can be contacted by mobile phones when a procedure is done, while video screens provide programmed videos and music to create a calming environment.
Practical, bright materials
Operational efficiency and flexibility were essential considerations during the planning of a facility of this scale, with very large departments. Keeping staff travel distances to a minimum meant looking at ways of keeping supplies, equipment, charting areas and waste disposal nearby, even as the utilisation of the departments rises and falls at different times of the day and week.
Being a military hospital, the finishes need to be very practical, durable and easy to clean. During exams, patient rooms require high light levels, with colour temperature that gives good colour rendering of the skin. Overall, the interior design of the new KHMC patient room reflects the state-of-the-art healthcare to be delivered, a contemporary international style, incorporating elements and materials that will make patients feel at home; mixing clean, bright materials with natural accents for contrast and depth; and referencing the diverse natural landscape and rich cultural heritage of Jordan.
The future
EBD is the future for the healthcare sector, a method, based on documented results, taking into account the emotional, psychological and physical wellbeing of the end user. The result is a dynamic space, directly catering to the needs of patients and those who treat them.
While it is still an area with many opportunities for exploration and research, there are numerous benefits to designs based on the already available EBD research. This research has shown that it saves time, avoids and decreases risk, improves the design process and creates modern, user-friendly spaces.
EBD is quickly gaining popularity within the wider design industry given its success in the healthcare sector. Other high-risk public spaces such as museums, universities and prisons are adopting this approach, providing informed design solutions where they matter most.
The post Evidence-based design in practice appeared first on Without Limits.
]]>The post Costing Mental Health Facilities appeared first on Without Limits.
]]>One in four people will experience a diagnosable mental health problem in any given year. The human and societal costs of those affected are immeasurable and the economic costs startling. All are equally unsustainable. Mental health problems represent the largest single cause of disability in the UK with an estimated cost to the economy of £105 billion a year.
Simon Stevens, Chief Executive of NHS England, commissioned a report by the independent Mental Health Taskforce that resulted in The Five Year Forward View for Mental Health, published in February 2016. The report identifies that a step change is needed to deliver improved access to high-quality care, more integrated services and a focus on prevention coupled with earlier interventions.
A coordinated and cohesive local approach
The implementation of The Five Year Forward View for Mental Health requires a coordinated and cohesive local approach. The responsibility for developing local plans lies with the Sustainability and Transformation Partnerships that were formed between local councils and the NHS across England in 2016 to develop integrated proposals to improve health and care.
Our mental health cost model report explores the evolving mental health landscape and government policy as the NHS is challenged to care for people with complex issues across the age spectrum, from young children through to older members of the population. It covers design guidance and technical standards, design considerations, lifecycle priorities, key cost drivers and a cost model based on a new-build 49-bed adult acute mental health facility in south-east England.
View and download the cost model here.
The post Costing Mental Health Facilities appeared first on Without Limits.
]]>